Globally, there is an undercurrent of contention about glaucoma; is it a back of the eye or front of eye issue? In whose territory does glaucoma treatment lie?
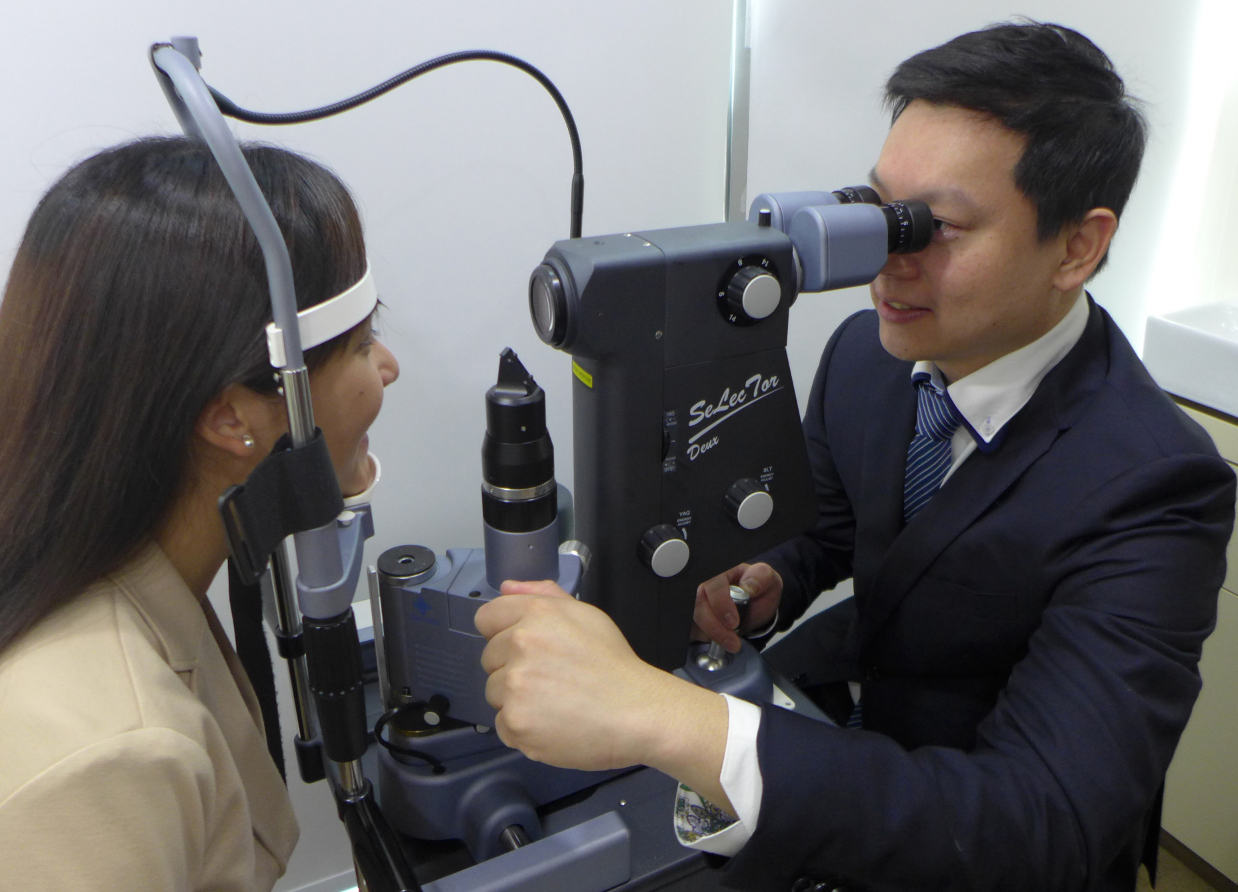
According to Dr. Kelvin Lee, MBBS, M.Med (Ophth), FRCS (Ed), FAMS, Director of Glaucoma Services at Eagle Eye Centre (EEC) Singapore, by definition, glaucoma is a back of eye problem.
“It’s a nerve disease,” said Dr. Lee. “It’s an optic neuropathy, resulting in characteristic visual field defects.”
However, if you break up glaucoma into its risk factors and treatments as well as the pathology, we realize the anterior chamber is very involved, said Dr Lee.
“For example, in angle closure, we perform laser iridotomy. Everything is happening at the front of the eye; there are no changes at the back of the eye yet, due to treatment.”
On the other hand, Professor Tina Wong BSc(Hons), MBBS, FRCOphth, FRCS(Ed), FAMS, PhD(Lond), senior consultant at the Glaucoma Department of Singapore National Eye Centre (SNEC), said that intervening early for patients at risk of angle closure can prevent angle closure attack in the first place.
“You’re breaking that pupil block mechanism from ever happening,’ she said. “These individuals don’t ever go on to develop a problem at the back of the eye.”
When asked about the front versus back of eye debate, Prof. Wong said: “Well, it’s both. The purists would say it’s a back of the eye condition, as per the traditional definition of a chronic, progressive optic neuropathy. But it’s not so black and white. You can’t categorically say it’s just an anterior segment disease, or it’s a posterior segment problem, because we treat the eyeball as a whole.”
However, Dr. Leonard Ang, MBBS, Doctorate Med, FRCS (Ed), MRCOphth (Lond), MMed (Ophth), FAMS (Ophth), medical director and senior consultant ophthalmologist at Lang Eye Centre, Singapore, is of the opinion that glaucoma is an anterior segment issue. He explained that the main risk factor and focus for treatment is the raised intraocular pressure (IOP).
“Intraocular pressure is a function of aqueous humor production by the ciliary bodies, and its drainage through the trabecular meshwork in the angle of the anterior chamber,” said Dr. Ang. “Primary glaucoma arises from functional or mechanical obstruction of the drainage passage.”
It gets interesting though, if you consider normal tension glaucoma – there is nothing wrong with the angles of these patients.
“The eye pressures are normal but there is an optic neuropathy similar to that in glaucoma patients with high pressures,’ said Dr Lee, who has a special interest in normal tension glaucoma.
Dr. Lee noted that normal tension glaucoma could possibly be attributed to problems with the vascular supply affecting the optic nerve. Another possible cause of normal tension glaucoma is also solely related to the back of the eye: “The nerve may be having a mechanical crush, due to the flexibility of the lamina cribosa,” he said.
However, though we can try to improve the circulation, the mainstay of treatment still involves lowering the IOP, as even at normal pressures the optic nerve in these patients is more sensitive to being crushed, explained Dr. Lee.
So, who should treat glaucoma?
In some countries, explained Dr. Kelvin Lee, unlike in Singapore, ophthalmological schools are more subdivided into anterior segment and back of the eye. This divide can cause a debate about who should treat a particular condition, like glaucoma.
Dr. Leonard Ang, based in Singapore, said that glaucoma is in the field of general ophthalmologists, regardless of subspecialty, but in cases of complex or refractory glaucoma, seeing a glaucoma specialist is advisable.
Meanwhile, Prof. Tina Wong explained that currently glaucoma treatments are focused at the front of the eye, targeting IOP via the trabecular meshwork outflow. But there is work being done on treatments targeting the back of the eye in glaucoma, for example, stem cells and optic nerve regeneration.
But, because you’re trying to regenerate something that is not really designed to regenerate, it’s hard to find therapies that work. So right now the mainstay of treatment is still lowering the raised intraocular pressure,” she said.