Thinking small appears to be the future direction for new ocular drug delivery systems, with methods like nanoemulsion, microemulsion, liposomes, nanoparticles, microspheres, inserts and collagen shields being investigated. Studies have demonstrated that these methods can improve pre-corneal residence time, increase ocular bioavailability and for some nanoparticle formulations, higher ocular penetration and drug availability have been shown. Some of the qualities of nanoparticles that are making it the new standout in ocular drug delivery is that due to their microscopic size, they do not cause eye irritation. Nanoparticles also have a positive surface charge, allowing a longer residence, and more absorption time on the negatively charged corneal surface.
Professor Krutika Sawant and colleagues from the Drug Delivery Research Laboratory, at The Maharaja Sayajirao University of Baroda in India, recently published their work in Materials Science and Engineering, and may have uncovered a way to deliver the pressure lowering efficacy of acetazolamide as a topical formulation, increasing ocular surface penetration and bioavailability right at the targeted tissue.
They started thinking small – nanoparticle small – and conducted in vitro and in vivo studies of ocular inserts impregnated with nanoparticles to topically deliver significant concentration of drug to the posterior segment. Precisely how small were their nanoparticles? The optimized formulations ranged from 367 nm± 8 nm….keep in mind that the diameter of a human hair is 75,000 nm!
“The positive surface charge of nanoparticles can allow a longer residence time to the corneal surface compared to classical eye drops as they interact with negatively charged cornea leading to slower ocular elimination rate, thereby enhancing corneal drug absorption,” the researchers explained.
Prof. Sawant’s ocular inserts of the nanoparticles (Eudraget) were created using a solvent diffusion nanoprecipitation method, which involves the dissolving of a polymer in an organic solvent and then desired particles are added to the solution before it is formed into the ocular insert.
The prepared ocular inserts were evaluated for thickness, content uniformity, folding endurance, disintegration time, morphology and stability.
“Overall, the inserts performed very well and in a lyophilized form, maintained stability for a period of 3 months,” reported the researchers.
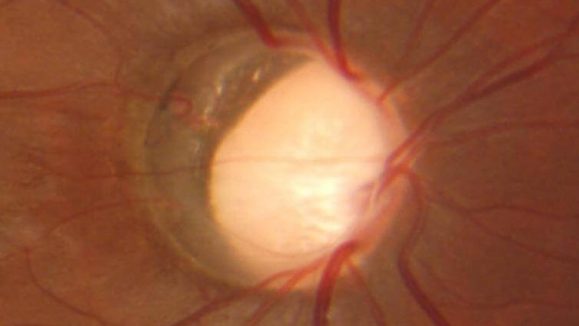
Once the inserts were confirmed to be structurally sound and uniform, then numerous parameters of the inserts and nanoparticles were assessed using both in vitro and in vivo animal models. The investigators looked at drug diffusion, trans-corneal permeability, ocular tolerability and IOP reduction study.
When compared with an acetazolamide suspension, the loaded nanoparticles exhibited better permeation and flux across corneal tissue, showed very good ocular tolerability in irritation studies and demonstrated a significant intraocular pressure lowering effect.
“The overall results obtained confirm that the nanoparticles impregnated ocular inserts can act as potential platform for drug delivery to the posterior segment of eye not only for glaucoma but also for other eye diseases,” concluded Prof. Sawant and colleagues.
Reference:
Rathod LV, Kapadia R, Sawant KK. A novel nanoparticles impregnated ocular insert for enhanced bioavailability to posterior segment of eye: In vitro, in vivo and stability studies. Mater Sci Eng C Mater Biol Appl. 2017;71:529-540.