Retinal experts shared tips for preventing hemorrhage and treating combined traction and rhegmatogenous retinal detachments, as well as the use of silicon oil in diabetic vitrectomy, on the second day of the APAO Congress.
Over the past years, advances in retinal surgery have made many formerly blinding conditions, such as diabetic retinopathy (DR), more manageable. Retinal experts shared their knowledge and experience for better surgical outcomes during the Retina (Surgical) Symposium on Diabetic Retinopathy and Retinal Vascular Diseases, held on February 24.
Preventing bleeding during surgery
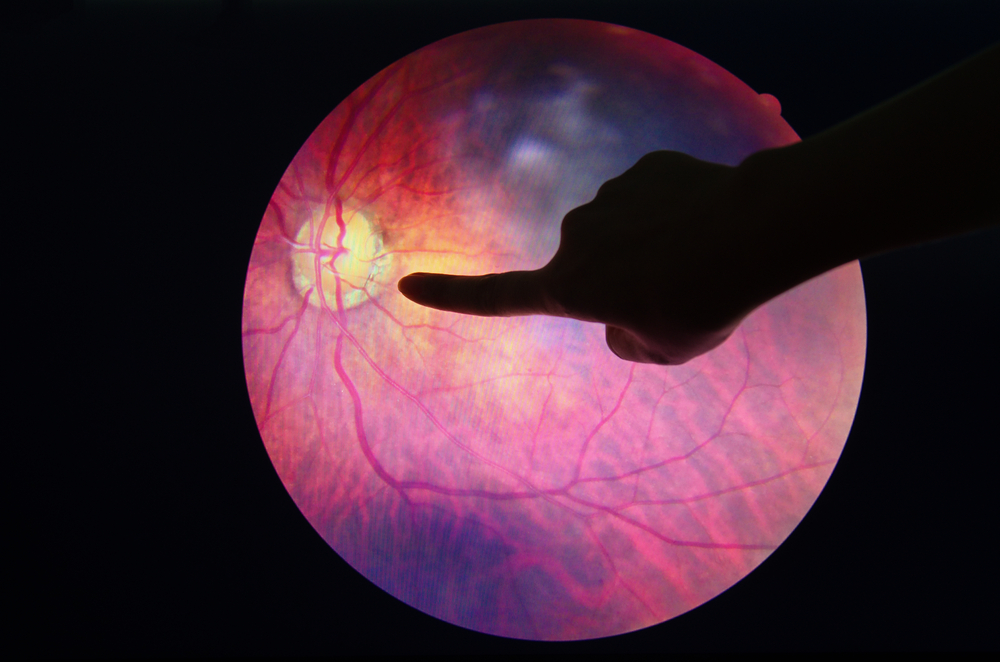
In proliferative diabetic retinopathy (PDR), severe vision loss can occur from complications of retinal neovascularization and fibrovascular proliferation. Even though these are indications for pars plana vitrectomy, intraoperative bleeding is very common, making surgical maneuvers very difficult because of poor visualization.
Postoperative vitreous cavity hemorrhage can occur in 20% to 30% of cases as well, noted Dr. Marie Joan Loy from the Philippines.
“Preoperative anti-vascular endothelial growth factor (anti-VEGF) injection is effective in regressing retinal neovascularization, thereby decreasing intraoperative and postoperative bleeding, complications, and surgical time, as well as improving surgical outcomes,” shared Dr. Loy. “Bevacizumab is the most studied anti-VEGF agent. A lower dose of bevacizumab (0.625 mg) appears to be effective and safe compared to higher doses,” she continued.
Dr. Loy also noted that studies have shown that injecting anti-VEGF six to 14 days pre-op significantly improved post-op best-corrected visual acuity (BCVA) and reduced recurrent vitreous hemorrhage and intraoperative bleeding.
“Doing surgery within six days of anti-VEGF injection appears better especially in young patients and in those with vitreous hemorrhage. Meanwhile, peri-operative use of anti-VEGF agents decreases the risk of early post-vitrectomy bleed, according to the Cochrane Database of Systemic Review,” she concluded.
Managing challenging retinal detachment
Meanwhile, Dr. Kian Seng Lim from Malaysia noted that combined traction and rhegmatogenous retinal detachments (TRD/RRD) are probably the most challenging surgical retinal cases.
“These are typically found in young diabetics with minimal PVD, which adds complexity to the surgery. Early surgical intervention is normally required,” he said.
“During surgery, I would attempt to remove as much posterior hyaloid as I could. The use of triamcinolone can be helpful,” Dr. Lim shared, adding that he pays meticulous attention to hemostasis throughout surgery as well.
“During surgery, retinal tears are usually found just adjacent to the fibrovascular stump. I attempt to release all tractions adjacent to retinal tears, which includes the fibrovascular tissue, posterior cortical remnant, and blood clots,” he continued. “My priority is to achieve macular attachment, firstly by releasing traction on the macula and optic disc, and secondly by releasing traction on the retinal tear. I believe that total dissection of fibrovascular tissue adds considerable risks to the surgery, and I avoid retinotomy and retinectomy at all costs.”
There have been numerous advancements in vitrectomy technology. “The discovery of anti-VEGF has made most of the complications in DR and TRD/RRD surgically treatable and with good outcomes,” he remarked.
Is silicone oil the best tamponade?
The prevalence of DR among people with diabetes in Asia ranges between 30% and 46% higher than in western countries, and Indonesia is one of the countries with the largest number of people with diabetes in the world, noted Dr. Referano Agustiawan from Indonesia.
“Various vitreous substitution with silicone oil and long-acting gas has been used during pars plana vitrectomy in cases with advanced diabetic complication. However, little clinical data are available regarding which vitreous substitute is best suited for this patient population,” he shared.
Dr. Agustiawan added that silicone oil promotes retinal reattachment by providing extended intraocular tamponade, compartmentalizes the eye, and confines angiogenic substances to the posterior segment, as well as acts as a diffusion barrier to oxygen — thereby preventing a decrease in anterior chamber oxygen tension after vitrectomy.
“Silicone oil tamponade is useful in severely diseased eyes with PDR, rubeosis, and previously failed vitrectomy,” he continued. “Silicone oil’s potential benefit is its stability inside the eye for up to a year, thus providing longer support to the retina and inhibiting the progression of neovascularization compared to other tamponades,” he said.
Nevertheless, silicone oil also has its disadvantages. Migration of silicone oil droplet into the retina and optic nerve can cause loss of myelinated optic nerve fibrosis, and there’s a risk of secondary glaucoma due to silicone oil droplet in the trabecular meshwork. Besides, there may be a need for a second surgery. In addition, silicone oil is associated with fibrovascular proliferation, has a lower surface tension, and is unable to completely fill the vitreous cavity.
“Although it remains inconclusive whether silicone oil is the best choice for diabetic vitrectomy, in my opinion, silicone oil is handy in complex cases of diabetic vitrectomy and cases of iatrogenic breaks that occur during surgery. Also, it should be used when one is less experienced or just starting with diabetic vitrectomy,” concluded Dr. Agustiawan.
Editor’s Note: The 38th Asia-Pacific Academy of Ophthalmology Congress (APAO 2023) was held on February 23 to 26 in Kuala Lumpur, Malaysia. Reporting for this story took place during the event. A version of this article was first published in Issue 3 of the APAO 2023 Show Daily.