There’s an established treatment available for chronic serous chorioretinopathy (CSCR), and that’s subthreshold laser (STL) therapy. If you were to stop reading in this sentence, you could leave with this takeaway: Yes, subthreshold laser therapy works for CSCR…
But you didn’t think we’d just say that and leave you to do all the guesswork, did you? Of course not. No, instead, we’re here today to discuss the findings and opinions presented by Dr. Alejandro Filloy Rius, a Spanish ophthalmologist who’s an excellent go-to guy for all things STL. Dr. Filloy presented his findings¹ at APAO 2023 in Kuala Lumpur, and there’s some significant good news in what he had to say.
For reference, CSCR affects the macula and can cause blurred vision due to fluid build-up beneath it. The condition usually affects one eye, although it might be present in both, and is more common in men than women. It further affects patients between the ages of 20 and 50, the most, and a personal history of stress is not unusual. While the more frequent non-chronic version may resolve on its own, the first “C” in CSCR means “chronic” which, well, means it’s an ongoing problem. Treatment in this condition is required in order to avoid long-term sequels.
CSCR overview
CSCR is a bit of an enigma in that it’s not exactly known why it occurs. However, Dr. Filloy explained that current evidence points to anomalies in the choroidal vessels that might cause a disruption in the retinal pigment epithelium (RPE), establishing a negative feedback loop resulting in the aforementioned fluid accumulation. If untreated, CSCR can lead to permanent vision quality loss in a number of ways, including blurring, distortion, blind spots, dulled color vision, and more. It’s a fairly prevalent condition, so it certainly deserves a place on the treatment development docket.
The most common treatment for CSCR until now has been photodynamic therapy (PDT) which is applied with its co-adjuvant, verteporfin. Most studies agree that STL and PDT are equivalent in results. However, while some papers suggest that PDT has the upper hand, Dr. Filloy rejects those claims. We’ll get to the why in just a moment.
There is another issue. There has been a worldwide shortage of verteporfin for around two years now, as Dr. Filloy noted, so alternative treatments are necessary. Currently, the shortage has caused a long line on PDT waiting lists, especially in certain countries, endangering the prognosis of these patients. While common knowledge does not yet support SLT over PDT, the evidence certainly appears to.
STL vs PDT
To be clear, let’s establish this: Dr. Filloy argues that STL is a viable alternative to PDT as a firstline treatment for CSCR. This is supported by the vast majority of the available literature. Regarding the evidence that argues in favor of PDT
(basically the PLACE trial)², Dr. Filloy has the following to say:
First, the main outcome presented in the pro-PDT papers² was the speed of the CSCR resolution, which Dr. Filloy believes to be not the most significant aspect regarding this disease; a slightly slower resolution will hardly impact the outcome of a long-ongoing condition. Second, and linked to the first one, the PLACE study itself finds there are no long-term significant differences in visual results. Third, the laser used was un-patterned. Fourth, few laser spots were applied in the
patients compared to what is known to be effective — only a fraction of what Dr. Filloy and most of the STL practitioners believe to be effective. These two last points (pattern and extension of treatment) suppose a violation of the cornerstones of an effective STL treatment. Naturally, these disagreements have led to some controversy.
New treatment requirements
So, if we were to have a new, better version of PDT that can treat then backlog of patients requiring CSCR treatment, it would have to have several features:
- It wouldn’t require verteporfin
- It would have to be cheap and readily available
- Patients would not need sun protection or home isolation afterwards
- It would need to be OCT/AF guided
- It would need to be easy to perform
- It would need to be free of described complications
- Retreatments would need to be available if necessary and, of course;
- It would need to be effective
And here’s where Dr. Filloy performs his a-ha moment: We have a treatment that ticks all of those boxes, and it’s STL.
Solid results for STL
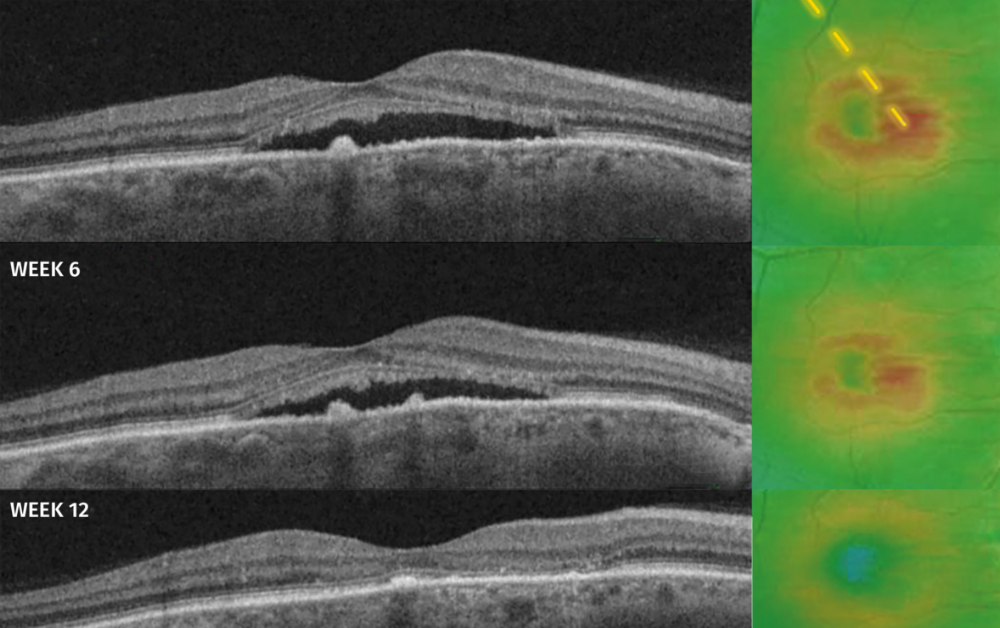
And here we enter the meat of Dr. Filloy’s case. He presented a prospective case series using an STL 577 nm yellow laser in a confluent extense pattern, is fovea-sparing and through individually-titrated power. He measured the effectiveness in terms of VA and subretinal fluid (SRF) resolution and looked on the changes in the choroidal structure. Follow-up was performed at 6, 12, and 24 weeks.
The study included 43 eyes from 37 patients, 75.7% of which were male.
The results were excellent: 93% of patients had improved conditions, showed some degree of improvement, 7% had stabilized, and 0% had worsened. Most patients — nearly 70% — experienced complete
resolution between 12 and 24 weeks. Choroidal thickness decreased significantly across the board as well.
A fine display
The evidence Dr. Filloy presented regarding the choroidal thinning shows that, indeed, STL does produce an anatomical response in treating CSCR (a kind of response also detected with PDT). Dr. Filloy convincingly argues that STL can be a solid first-line defense for CSCR, especially in light of the ongoing shortage of verteporfin.
At this point, however, astute readers may have stopped and asked, “Well wait…just how does it work?”
This is a good question, and like CSCR itself, just how STL works remains a bit of an enigma. However, Dr. Filloy has some suggestions.
Most importantly, as Dr. Filloy explained, “The anti-inflammatory cascade elicited by the subthreshold laser stimulus might “disrupt that disruption”, thus “resetting” the RPE. However, the reason behind the choroidal thinning remains unclear, though it may be due to a two-way mechanism.
Given the circumstances and evidence provided by Dr. Filloy, STL represents a significant step forward in treating CSCR. With the current backlog of patients waiting to be treated, a novel treatment for the condition is just what the doctor ordered.
We look forward to more data coming out regarding the fisiopathological pathways of STL, but the important thing for now is that it’s clear it does indeed work. Kudos to Dr. Filloy and his team for the findings, and we can’t wait to see what’s next.
In the meantime, check out Lumibird® Medical’s site at www.subliminal-laser-therapy.com to find out more exciting developments.
[Editor’s Note: The 38th Asia-Pacific Academy of Ophthalmology Congress (APAO 2023) was held on February 23 to 26 in Kuala Lumpur, Malaysia. Reporting for this story took place during the event. A version of this article is included in PIE Magazine issue 28]
References
- Torrellas B, Filloy A, Wu L, Chhablani J, Romero-Aroca P. Effectiveness, Safety and Choroidal Changes of a Fovea-Sparing Technique for the Treatment of Chronic Central Serous Chorioretinopathy with Yellow Subthreshold Laser. J Clin Med. 2023;12(3):1127.
- van Dijk EHC, Fauser S, Breukink MB, et al. Half-Dose Photodynamic Therapy versus High-Density Subthreshold Micropulse Laser Treatment in Patients with Chronic Central Serous Chorioretinopathy: The PLACE Trial. Ophthalmology. 2018;125(10):1547-1555.
Editor’s Note: A version of this article was first published in PIE Magazine Issue 28.