Blockbuster meds, blockbuster risks? Trending GLP-1s (like Ozempic) are now raising red flags for nAMD.
A new population-based cohort study has found that patients with diabetes who use glucagon-like peptide-1 receptor agonists (GLP-1 RAs)—a drug class that’s taken center stage in both diabetes and weight-loss treatment—may face a significantly higher risk of developing neovascular age-related macular degeneration (nAMD).
The research, published in JAMA Ophthalmology and led by Dr. Reut Shor and colleagues, analyzed data from 139,002 patients aged 66 years or older with diabetes in Ontario, Canada. The study compared 46,334 patients who had been exposed to GLP-1 RAs for at least six months with 92,668 matched patients who had not.1
Over a mean follow-up period of 2.4 years, researchers found that patients taking GLP-1 RAs had more than double the risk of developing nAMD compared to their unexposed peers. The adjusted hazard ratio came in at 2.21; a number that may prompt a few raised eyebrows in both retina and diabetes clinics.1
READ MORE: New Data Links Ozempic to Rare Blinding Disease; Denmark Calls for Probe
“The incidence of nAMD was higher among the exposed cohort than among the unexposed cohort,” the authors reported. Among those taking GLP-1 RAs, 0.2% developed nAMD, compared to 0.1% in the unexposed group.1
The longer, the riskier?
The study also found that the longer patients were on GLP-1 RAs, the greater the risk appeared to be. Those on medication for more than 30 months had the highest risk, suggesting that duration of exposure may play a role.1
Most patients in the GLP-1 RA group (97.5%) were taking semaglutide, the blockbuster drug that has dominated both headlines and pharmacy shelves in recent years. A much smaller portion was on lixisenatide.1
READ MORE: EMA Announces Start of Semaglutide Investigation
What’s behind the link?
The researchers offered several possible biological explanations. One is that GLP-1 RAs cause rapid drops in blood glucose levels, potentially creating a hypoxic environment in the retina, which is an ideal setting for abnormal angiogenesis to take hold.1
Another theory? GLP-1 RAs might increase levels of chemokine CXCL12, which can boost vascular endothelial growth factor (VEGF) expression under hypoxic conditions, nudging the eye toward neovascular mischief.1
A pattern emerges
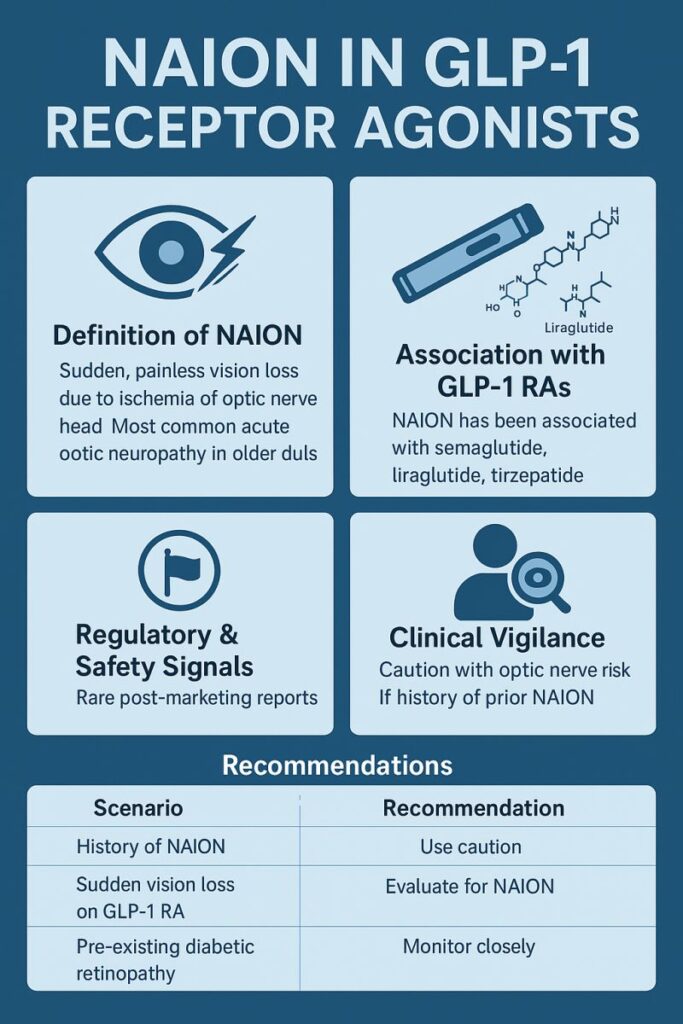
In an accompanying editorial, Dr. Brian L. VanderBeek noted that these findings echo a broader conversation about GLP-1 RA-associated eye complications. Past reports have linked this drug class to worsening diabetic retinopathy and nonarteritic anterior ischemic optic neuropathy (NAION).
While Shor et al. referred broadly to GLP-1 RAs, Dr. VanderBeek pointed out the dominance of semaglutide in the exposed cohort. “Semaglutide has been suggested to be the drug most associated with ocular adverse events,” he wrote.2
Dr. VanderBeek also highlighted the real-world implications: even if the absolute risk difference is small (0.11%, or roughly 1 in 1,000 users), the soaring popularity of these drugs could result in a notable number of new nAMD cases over time.2
READ MORE: Bayer Notches Dual EYLEA 8mg Wins With China nAMD Approval and EU 6-Month Interval Extension
A balancing act for clinicians
To be clear, GLP-1 RAs offer well-documented benefits: cardiovascular, renal and metabolic among them. But eye care professionals may want to keep this potential risk on their radar, particularly for patients with longer exposure durations or existing retinal concerns.
“Further research is needed to elucidate the exact pathophysiological mechanisms involved and to understand the trade-offs between the benefits and risks of GLP-1 RAs,” the study authors concluded.1
Dr. VanderBeek echoed the call for more research and stressed the importance of identifying which patients may be most vulnerable, especially as GLP-1 RAs expand their footprint beyond diabetes into weight management and other indications.2
Editor’s Note: This content is intended exclusively for healthcare professionals. It is not intended for the general public. Products or therapies discussed may not be registered or approved in all jurisdictions, including Singapore.
References
- Shor R, Mihalache A, Noori A, et al. Glucagon-Like Peptide-1 Receptor Agonists and Risk of Neovascular Age-Related Macular Degeneration. JAMA Ophthalmol. 2025:e251455. [Epub ahead of print.]
- VanderBeek BL. Should We Be Concerned About Glucagon-Like Peptide-1 Receptor Agonists? JAMA Ophthalmol. 2025 Jun 5. [Epub ahead of print.]
![[Newsroom] Thumbnail GLP1 and AMD Story](https://piemagazine.org/wp-content/uploads/sites/4/2025/06/Newsroom-Thumbnail-GLP1-and-AMD-Story.png)