There’s few things worse than a migraine, as sufferers know well. The distinct pain and disturbing symptoms can be debilitating and drastically affect a person’s quality of life. Even infrequent migraines can be inconvenient, to say the least, whereas frequent migraines can lead a person to try all sorts of potential cures.
The term “ophthalmic migraine” refers to any migraine affecting the eyes, and includes visual symptoms. It’s a bit of a misnomer since it doesn’t have anything to do with surgery. They’re often referred to as ocular migraines or visual migraines, since the pain can often feel like it’s located in one or both eyes. Visual disturbances are fairly common, and fairly disturbing.
While the exact causes and symptoms vary from person to person and even migraine to migraine, there are some commonalities that can be explored. So, let’s check out the causes, symptoms, and potential preventions and treatments for ophthalmic migraine headaches.
What Causes Ophthalmic Migraines?
If we could tell you point blank what causes migraines in general we’d be millionaires. The exact causes are always a bit mysterious to both doctors and patients. People who suffer from ophthalmic migraines often have suffered from traditional, chronic migraine headaches, so the two are linked. That doesn’t necessarily mean they’re fully understood, however.
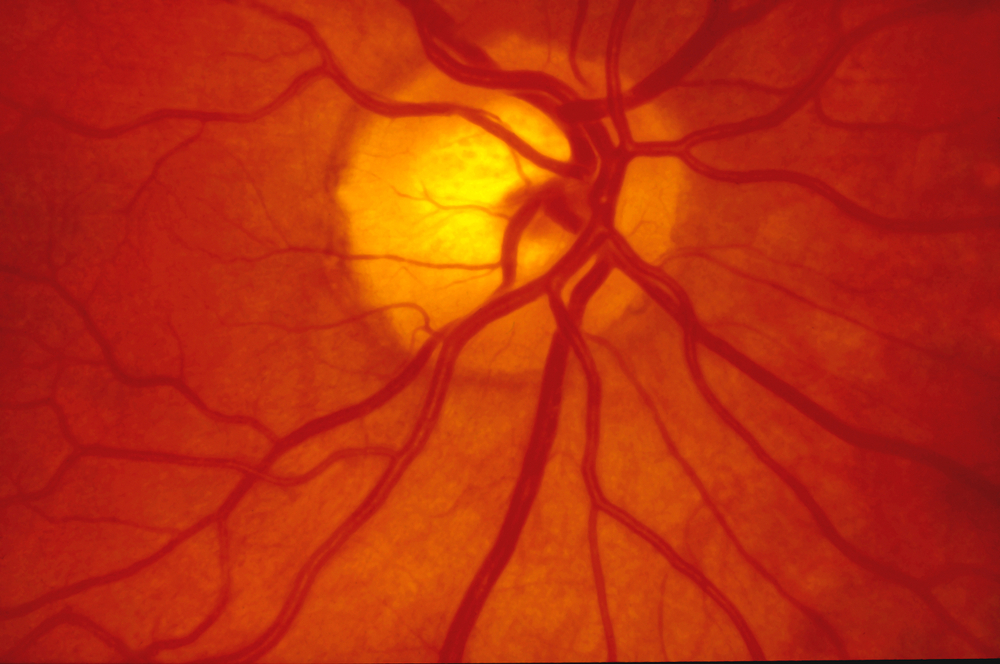
The apparent cause of ocular migraines is vasospasm of the ophthalmic artery and retinal blood flow. The narrowing of the blood vessels reduces blood to the eyes which can lead to the visual symptoms unique to ocular migraines.
So, we’ve got a general idea of what causes an ophthalmic migraine: reduced blood flow due to blood vessels acting up. Ok, great. But what causes that?
Herein lies the mystery. There is a broad host of potential triggers, which are usually unique to an individual. What triggers a migraine for one patient might not for another. Your eye doctor or general practitioner may help you identify some triggers. Women tend to suffer from migraines at a rate of around three times that of men. If you suffer from chronic migraine headaches, you should note your circumstances before the migraine begins.
Triggers can include:
- Certain foods and drinks, including (sadly) red wine, or food additives like monosodium glutamate or nitrates
- Emotional stress
- High altitudes
- Screen use or eye strain
- Oral contraceptives
- Exercise
- Dehydration
- Smoking
- Overheating (hyperthermia)
- Low blood sugar
Identifying your triggers can be difficult, but documenting details before a migraine can help you figure out what sets you off. Note the time of day, what you’ve eaten in the last 24-48 hours, how long the migraine lasts, how it feels, where the migraine is on your head, any visual effects, potential sources of stress, or anything else you think might be relevant. In worst-case scenarios, consistent migraines may represent an underlying systemic problem like lupus or antiphospholipid syndrome.
Ophthalmic Migraine Symptoms

Of course, migraines usually mean headaches. But we’re here to discuss the visual effects experienced which, believe it not, do not always come associated with headaches. Common visual symptoms include dimmed vision and seeing squiggly or zig-zag lines, blind spots, flashing lights, or twinkling stars. There are generally two types of ocular migraines: Aura migraines and retinal migraines. Of the two, retinal migraines are more serious.
A retinal migraine can lead to an apparent dimming of vision. This can be accompanied by twinkling lights and even temporary blindness. The symptoms can occur in one or both eyes and generally dissipate within a matter of hours. If you experience these symptoms, it’s important to speak to a doctor as soon as possible as retinal migraines can potentially lead to irreversible vision loss.
Migraines with aura have visual symptoms like those mentioned above including visual loss, and can include a number of different visual patterns. The visual aspect of the migraine aura usually occurs before the headache begins, and continues until the peak of the migraine’s pain. Do note that not all patients experience a headache concurrent with visual aura symptoms, though the symptoms are often an indicator that a migraine episode is on its way.
Preventing or Treating Ophthalmic Migraines

There are many different ways to prevent or treat ophthalmic migraines, so patients will need to figure out what works best for them. Preventive treatments can include noting triggers and avoiding them, though this practice may take some time to be refined. Ideally, migraines should be prevented entirely. Resting your eyes by looking at something other than screens, when possible, can be helpful.
Medical treatments can include NSAIDs like ibuprofen, aspirin, or acetaminophen as well as drugs like verapamil, propranolol, and nifedipine. Of course, nothing beats a doctor’s advice since it’s custom tailored to the patient.
If you’re experiencing visual disturbances, an ophthalmologist or general practitioner may determine that a trip to the neurology department is the best way forward.
It may be some time yet until we determine what really causes migraines, and the controversy is likely to remain. What we do know for sure, however, is that they’re absolutely no fun. Any visual symptoms associated with migraines should be taken seriously and quickly treated. After all, headaches are bad enough as is. Who wants vision loss to go with them?



