When 382 million people globally are currently suffering from diabetes mellitus (DM) and the number projected to reach 592 million by 2035, the treatment burden of diabetic macular edema (DME) which is the main cause for vision loss in DM patients increases tremendously. What is more challenging is the persistence of DME which seem to elude treatment, perhaps due to its complex pathogenesis.
On the horizon, new agents are emerging for the treatment of persistent DME. Apart from the breakthrough anti-VEGFs in treating center-involving DME, researches have explored corticosteroids, laser and surgery, and now; a paper has reviewed novel options like new anti-VEGFs, interleukin inhibitor, Rho-kinase inhibitor, and neuroprotective agents.
Multifactorial Pathogenesis
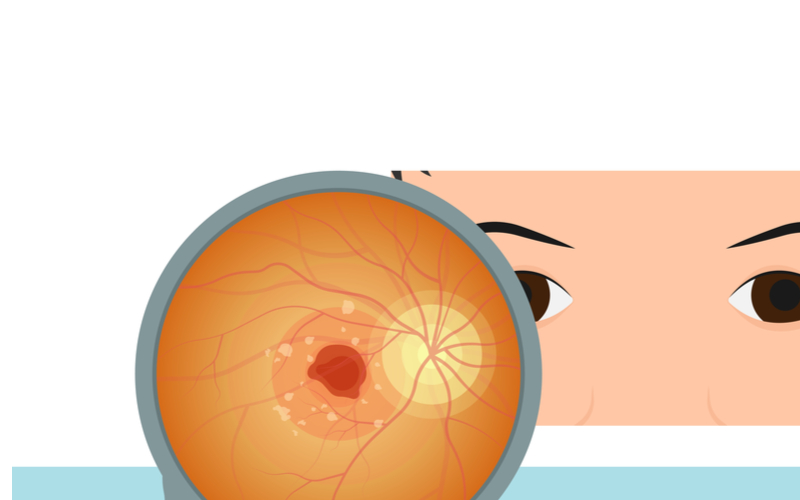
DME’s pathogenesis is known to be multifactorial with increased oxidative stress, inflammation, vascular dysfunction and neurodegeneration being suggested as newer contributing factors of its development.
A recently published review1 expounded on multiple biochemical pathways which are important players in the formation of DME. The pathways include the up-regulation of VEGF, placental growth factor (PIGF), angiopoetin-2 (Ang-2), intercellular adhesion molecule (ICAM-I), interleukins, pigment epithelium-derived factor, matrix metalloproteinases, prostaglandins, and other types of cytokines.
Recent studies also propose that the change in the neurovascular unit which includes Muller cells, astrocytes, ganglion cells, and pericytes contribute towards DME’s pathology.2
New Treatments on the Block
Novel anti-VEGF agents with “longer duration of action” could lessen the frequency of injections and patients’ economic burdens.
One is conbercept, a recombinant fusion protein designed as a receptor decoy with “high affinity for all VEGF isoforms and PIGF. The PHOENIX study3 investigated conbercept’s efficacy and safety for neovascular age-related macular degeneration (nAMD), finding that there were significant benefits visually and anatomically with three initial monthly doses of conbercept (loading dose) followed by a quarterly dosing of conbercept.
Based on the HAWK and HARRIER studies4, a molecularly lightweight “humanized single-chain variable (scFc) antibody fragment VEGF inhibitor called brolucizumab has been approved in the United States to treat nAMD. This newbie is showing “comparable visual gains” similar to aflibercept “with greater retinal fluid resolution”. However, a study by Baumal et al.5 involving 15 eyes from 10 practices had shown retinal vasculitis and intraocular inflammation within the first three months of its availability.
Next, the use of the novel faricimab addresses the angiogenic factor and inflammatory cytokines which were not focused on with the use of previous anti-VEGFs. It is designed for intraocular use specifically to inhibit both VEGF and the Ang-2 pathways. It was reported in phase 2 of the BOULEVARD study6,7 that patients had “superior gains in visual acuity” compared with ranibizumab when administered with 6 mg intravitreal faricimab monthly for 20 weeks.

Customized Delivery
Aside from anti-VEGF agents, the review also looked at the port delivery system(PDS) as a “novel, innovative, long-acting drug delivery system” that continuously delivers “a customized formulation of ranibizumab into the vitreous”. Permanent and refillable, the implant which forms the PDS enables ranibizumab to be passively diffused from a reservoir, going into the vitreous cavity. It is also a sutureless implantation in a “self-retaining” procedure. The LADDER study8,9 showed a refill time of 15 months where 80% of patients did not need refills for the first 6 months. Results of its visual acuity and anatomic outcomes matched the ones from monthly intravitreal ranibizumab.
Abicipar Pegol
Drawing from the common protein patterns in nature – the ankyrin repeats – researchers have created “libraries of artificially stacked designed ankyrin repeat proteins (DARPin) which are a new class of proteins that specifically enjoins itself to only certain proteins. The PALM study10-12 looked at the abicipar pegol, a specifically-designed DARPin that binds and inhibits VEGF and it reported improvements in visual acuity.
Interleukin Inhibitors and Chemokine Inhibitors
As recent studies showed the increased presence of inflammatory cytokines like IL-1 and IL-6 in the vitreous of DME patients, the use of IL-1 receptor antagonists seem to be promising.13 Tested on bovine retina, the trial saw a reduction in “glucose-induced abnormalities”. The R07200220 recombinant fully humanized immunoglobulin G2 (IgG2) isotype monoclonal antibody that binds IL-6 and stops all forms of IL-6 signalling is designed to treat DME, uveitic macular edema and nAMD.
In a similar way, Rho-kinase inhibitors can add to the efficacy of anti-VEGF treatment of persistent DME.14 Aeri Pharmaceuticals (New Jersey, USA) has designed “a sustained-release intravitreal implant” that fights against nAMD and DME by inhibiting the Rho-kinase and protein kinase C.
Neuroprotective Measure
After being discovered that neurodegeneration occurs early in the pathogenesis of DR and DME, drugs that protect the retinal nerves like topical brimonidine and somatostatin were studied in the EUROCONDOR trial.15 The results showed that although they weren’t efficacious in “preventing the development of neurodegeneration”, these agents somehow prevented the further progression of neurodegeneration in patients.
The review suggested that it was vital to examine the different components that had contributed towards DME’s complex pathogenesis in order to come up with personalized treatment plans for each patient. This could lead to a future of “individualized management of DME” involving the above agents.
References:
- Kuroiwa DAK, Malerbi FK, Regatieri CVS. New Insights in Resistant Diabetic Macular Edema. Ophthalmologica. 2021;244(6):485-494.
- Das A, McGuire PG, Rangasamy S. Diabetic macular edema: pathophysiology and novel therapeutic targets. Ophthalmology. 2015;122(7):1375–1394.
- Liu K, Song Y, Xu G, Ye J, Wu Z, Liu X, et al. Conbercept for treatment of neovascular age-related macular degeneration: results of the randomized phase 3 PHOENIX Study. Am J Ophthalmol. 2019;197:156–167.
- Dugel PU, Singh RP, Koh A, Ogura Y, Weissgerber G, Gedif K, et al. HAWK and HARRIER: ninety-six-week outcomes from the phase 3 trials of brolucizumab for neovascular age-related macular degeneration. Ophthalmology. 2021;128(1):89–99.
- Baumal CR, Spaide RF, Vajzovic L, Freund KB, Walter SD, John V, et al. Retinal vasculitis and intraocular inflammation after intravitreal injection of brolucizumab. Ophthalmology. 2020;127(10):1345–1359.
- Sharma A, Kumar N, Kuppermann BD, Bandello F, Loewenstein A. Faricimab: expanding horizon beyond VEGF. Eye. 2020;34(5):802–804.
- Sahni J, Patel SS, Dugel PU, Khanani AM, Jhaveri CD, Wykoff CC, et al. Simultaneous inhibition of angiopoietin-2 and vascular endothelial growth factor-A with faricimab in diabetic macular edema: BOULEVARD phase 2 randomized trial. Ophthalmology. 2019;126(8):1155–1170.
- Sharma A, Kumar N, Parachuri N, Kuppermann BD, Bandello F, Regillo CD. Ranibizumab port delivery system (RPDS): realising long awaited dream of prolonged VEGF suppression. Eye. 2020;34(3):422–423.
- Sharma A, Kumar N, Kuppermann BD, Francesco B. Re: Campochiaro, et al: The port delivery system with ranibizumab for neovascular age-related macular degeneration: results from the randomized phase 2 Ladder clinical trial (Ophthalmology. 2019;126:1141–1154). Ophthalmology. 2019;126(11):e87–88.
- Agarwal A, Afridi R, Hassan M, Sadiq MA, Sepah YJ, Do DV, et al. Novel therapies in development for diabetic macular edema. Curr Diab Rep. 2015;15(10):75.
- Sadiq MA, Halim MS, Hassan M, Onghanseng N, Karaca I, Agarwal A, et al. Pharmacological agents in development for diabetic macular edema. Int J Retina Vitreous. 2020;6(1):29–11.
- Shah SU, Maturi RK. Therapeutic options in refractory diabetic macular oedema. Drugs. 2017;77(5):481–492.
- Figueras-Roca M, Molins B, Sala-Puigdollers A, Matas J, Vinagre I, Ríos J, et al. Peripheral blood metabolic and inflammatory factors as biomarkers to ocular findings in diabetic macular edema. PLoS One. 2017;12(3):e0173865.
- Minami Y, Song YS, Ishibazawa A, Omae T, Ro-mase T, ishiko S, et al. Effect of ripasudil on diabetic macular edema. Sci Rep. 2019;9(1):3703–9.
- Simó R, Hernández C. Neurodegeneration in the diabetic eye: new insights and therapeutic perspectives. Trends Endocrinol Metab. 2014;25(1):23–33.