- COVID-19 causes a number of symptoms beyond the classic signs of a dry cough, fever and anosmia.
- A number of reports have emerged of patients suffering from blurred vision in conjunction with the coronavirus.
- This, and other signs, is a classic indicator of central retinal vein occlusion.
Novelty is often the spice of life and new things and ideas are always welcomed by the Media MICE team. We do enjoy reading and writing about the latest developments in ophthalmology and the same applies to rare conditions or variants of already existing ones. Of course, one must do this with a degree of sympathy and remember that behind the case study is a real patient with real health issues.
So when we started researching some novel aspects of COVID-19 and its ophthalmological consequences we became very interested. We recently published an article about how visual hallucinations have increased in sufferers of Charles Bonnet syndrome thanks to the isolation caused by coronavirus-related lockdowns. We also discovered cases where patients were affected by central retinal vein occlusion (CRVO) due to COVID-19 infection.
CRVO occurs when the main vein that drains blood from the retina closes off partially or completely, causing blurred vision and other issues. This distorted vision is due to swelling of the macula and can be severe, however other patients may experience a waxing and waning of their symptoms, which is called transient visual obscurations. If the patient has other eye conditions such as glaucoma they are more likely to experience severe symptoms combined with pain, redness, irritation and other problems.1
Surgery at the Sheikh’s
The specific cause of CRVO is often unknown, however it is more frequently encountered in patients with high blood pressure and diabetes. These are both high-risk factors for severe COVID-19 infection, as is obesity. While that might appear to make infection with the coronavirus variant combined with CRVO likely, it has been described as “a novelty” and is relatively rare.
Bilateral Central Retinal Vein Occlusion in a 40-Year-Old Man with Severe Coronavirus Disease 2019 (COVID-19) Pneumonia2 is a case study that offers excellent insight into the classic example of CRVO combined with COVID-19. The group of researchers behind the study is based in the United Arab Emirates at the Sheikh Khalifa Medical City in the country’s capital, Abu Dhabi. The 40-year-old patient presented with classic coronavirus symptoms including a three-day history of shortness of breath, cough and fever.
The patient’s medical history showed hypertension and morbid obesity, and also reported blurring of vision. He underwent high-resolution tomography of the chest, a right leg deep venous thrombosis on Doppler ultrasonography, and after a fundal examination was diagnosed with CRVO. The patient was treated with full-dose anticoagulation and discharged on rivaroxaban for three months, with his vision returning to near normal after a period of two weeks.2
From the Middle East to Europe and Back Again
CRVO and COVID-19 patients will not always be morbidly obese, and indeed, may not possess any serious risk factors. A 54-year-old patient in Milian, Italy, presented to doctors complaining of scotomas and decreased vision in her right eye. She had COVID-19-related pneumonia but had no risk factors other than a transient hyper-coagulability status likely related to the ongoing infection.
After funduscopic examination and multimodal imaging, the patient was revealed to have rare retinal hemorrhages, retinal whitening and a fern-like hypo-autofluorescent appearance typical of CRVO. The Italian doctors differed from their Emirati colleagues by treating their patient with systemic steroids treatment which normalized her inflammatory and coagulation status. Happily, her vision returned to normal and the occlusion was resolved.3
CRVO caused by COVID-19 infection is a novelty in that it is rare but it has occurred often enough for clinicians to take serious note. When a 33-year-old Israeli patient presented with blurred vision in his left eye for over a month, accompanied by flashes of light without any accompanying neurological symptoms, he was diagnosed with CRVO as well as coronavirus. After a month, the patient enjoyed a complete resolution of symptoms and a gradual improvement of retinal vascular appearance.4
The authors of the Israeli patient case study concluded that “to the best of our knowledge this is the first report of CRVO in association with COVID-19.” Since they made their report more cases have occurred, and in fact, we only highlighted three among many on PubMed and other research sites. While it is indeed a novelty, and rare, the complications of COVID-19 should also include potential CRVO.
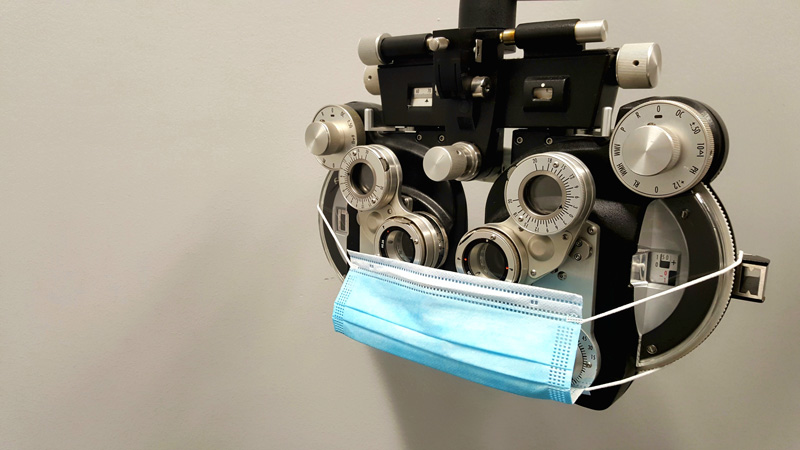
Therefore, it is recommended that clinicians bear in mind potential co-infection with COVID-19 when symptoms of CRVO occur in their patients. Maintaining social distancing and proper sanitization measures becomes far more important than usual in this scenario. As COVID-19 continues to mutate other co-morbidities and co-infections may occur, so it would be best to exercise a degree of caution with regard to new viral developments.
References:
- The American Society of Retina Specialists. Central Retinal Vein Occlusion. Available at https://www.asrs.org/patients/retinal-diseases/22/central-retinal-vein-occlusion. Accessed on April 1, 2021.
- Gaba WH, Ahmed D, Al Nuaimi RK, et al. Bilateral Central Retinal Vein Occlusion in a 40-Year-Old Man with Severe Coronavirus Disease 2019 (COVID-19) Pneumonia. Am J Case Rep. 2020;21:e927691.
- Invernizzi A, Pellegrini M, Messenio D, et al. Impending Central Retinal Vein Occlusion in a Patient with Coronavirus Disease 2019 (COVID-19). Ocul Immunol Inflamm. 2020;28(8):1290-1292.
- Yahalomi T, Pikkel J, Arnon R, Pessach Y. Central Retinal Vein Occlusion in a Young, Healthy COVID-19 Patient: A Case Report. Am J Ophthalmol Case Rep. 2020;20:100992.




Happened to me.The retina specialist said It’s caused by diabetes, high blood pressure or cholesterol. All my tests came back normal. Now I get shots in my eye every month for the last 4 months. It started 4 days after my first vaccination with the Pfizer vaccine. I started seeing flashes in the morning for approximately 15 minutes. After 3 weeks it progressed into a fog, that’s when I called the eye doctor. They told me I needed to see an eye surgeon who told me I needed to see a retina specialist.
I had the same problem. I had CRVO after Pfizer booster vaccine. I have been given injection for the past 4 months. I had COVID-19 three weeks ago. My condition turned worse. Retinal specialist is going to give me some stronger medicine. This is really a bad situation to be in.
I also was diagnosed with RVO a couple of months after my second pfyzer vaccine. The specialist thought it had started a couple of months earlier I didn’t realise as my other eye was compensating. I have had 3 lots of injections which have helped so far. I dont know whether I should have my booster vax although I am now on aspirin which I thought my help as a preventative.
Same thing happened to me as well. Two days after the second pfizer shot, I noticed a grey blind spot in the center of vision in my right eye (the left eye is unaffected). It lasted for few minutes and happened 2-3 times a day for few days. The following weeks and months, the vision started to slowly become blurry and became sensitive to bright light and experienced morning flashes. I then consulted an eye doctor and was diagnosed with CENTRAL RETINAL VEIN OCCLUSION in the right eye. The doctor referred me to eye surgeon and also asked me to see… Read more »
Another case here. I don’t think I ever had COVID, definitely not symptomatic. No significant cardiovascular risk factors. But had some visual symptoms 5 months after the second Pfizer shot, and was diagnosed with CRVO about a month after that. It was mild for the first couple months, just worsening gradually, eventually to the point of major blurriness and edema. Received one shot of the anti-VEGF treatment so far.
This happened to me 3 months post covid at 40yrs old. Extremely rare for my age. Every test imaginable was run, mri/contrast mri, ct, bloodwork multiple times – no issues whatsoever. Thankfully, I responded well to monthly shots and am now basically in “remission” for lack of a better term. At my last appt with the retinal doc he said he was finally ready to call this a covid-induced event.