Singaporean ophthalmologists discussed new technologies and methods that could change disease diagnosis and management during the 5th ASEAN Ophthalmology Society Virtual Congress (AOS Virtual 2022).
Real-time Intraoperative OCT
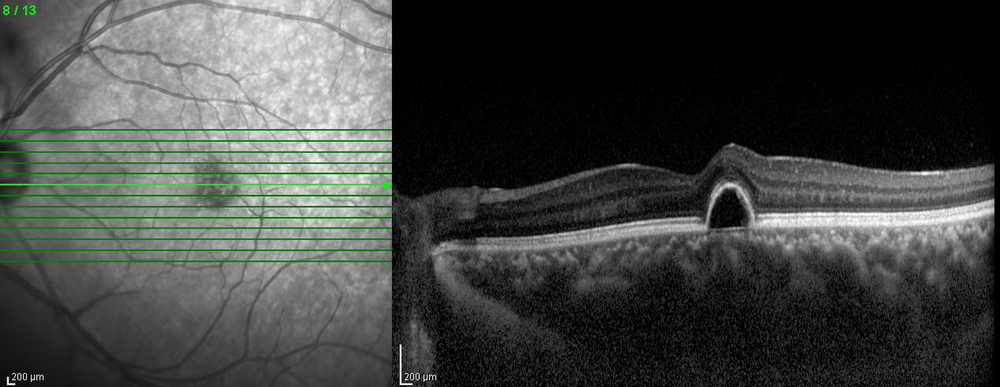
Optical coherence tomography (OCT) has revolutionized the diagnosis of eye disease and patient management since 1993 when the first OCT retinal imaging prototype instrument was created. In 2006, the spectral-domain OCT (SD-OCT) became the standard of care. Later, new technologies were born, such as the swept-source OCT (SS-OCT) and OCT angiography. “With the integration of the OCT into the microscope, for the first time, real-time OCT was possible. Today, there are three FDA-approved intraoperative OCT (iOCT) systems – the ZEISS Rescan 700, Haag-Streit iOCT and Leica EnFocus,” noted Dr. Tien-En Tan from Singapore.
He shared his knowledge and experience of using the Leica EnFocus iOCT, which had helped altered decision-making in surgeries. “The Leica EnFocus is fully integrated into the Proveo 8 Opthalmic Microscope. It is a spectral domain OCT and can be used on the anterior and posterior segments. It has an axial resolution of 2.4-4.0 μm, high scan density of 500-1000 B-scans and automatic image optimization,” he said.
In the DISCOVER study* of 593 posterior segment cases, it has been shown that iOCT added valuable information in about 60% cases, altered surgical decision-making in about 30% of the cases, and was most useful for membrane peeling (there was 20-40% discordance between surgeon impression and iOCT findings on whether the membrane peel was complete).
He shared a case done in the Singapore National Eye Centre where the iOCT helped to detect extrafoveal polypoidal choroidal vasculopathy (PCV), which helped the surgeon to decide on performing an intraoperative endolaser. “This step would not be possible without the iOCT,” he said.
According to Dr. Tan, various applications for iOCT in vitreoretinal surgery had been described, including epiretinal membranes, membrane peeling, macular holes, retinal detachment, vitreous hemorrhage, diabetic vitrectomy, pediatric vitreoretinal surgery, and subretinal surgery.
In the future, OCT-compatible surgical instruments may be available as there have been attempts in developing them, to rectify the issue of shadowing on the OCT caused by current surgical instruments, noted Dr. Tan. “Other possibilities in the future include automated iOCT tracking, and digital staining as the software improves,” he said.
Use of the RNFL Thickness to Detect Early Glaucoma
A diagnostic challenge in using OCT to detect early glaucoma exists as anatomical factors can affect retinal nerve fiber layer (RNFL) measurements, according to Dr. Jacqueline Chua Yu Min from Singapore. “Clinically, there’s a need for a single, comprehensive model to account for all factors that is associated with RNFL thickness, such as ethnicity, age, refractive error, among others, to improve the diagnostic performance of OCT for early glaucoma detection,” she said.
Dr. Chua and her colleagues developed a compensation model with the aim of refining and validating an Asian-specific compensation model based on their established regression model (Caucasian-model).
“We hypothesize that the refined model will further reduce the inter-subject variability of the circumpapillary RNFL thickness,” she added.
Two thousand six hundred ninety-nine (2,699) healthy participants were enrolled to construct and test a multivariate compensation model, which then was applied in 387 healthy participants and 387 patients with glaucoma. Compensated RNFL thickness was generated based on ethnicity, age, refractive error, optic disc (ratio, orientation, and area), fovea (distance and angle), and retinal vessel density.
After applying the Asian-specific compensation model, the standard deviation of RNFL thickness reduced, with the greatest effect seen on Chinese participants (16.9%), followed by Malay participants (13.9%), and Indian participants (12.1%). Multivariate normative comparison outperformed measured RNFL for discrimination of early glaucoma (Area under the curve [AUC], 0.90 vs. 0.85; P < 0.001), moderate glaucoma (AUC, 0.94 vs. 0.91; P < 0.001), and advanced glaucoma (AUC, 0.98 vs. 0.96; P < 0.001).
“Compensation model improves the diagnostic performance of RNFL measurements. Compared to deep learning approaches, the current technique is a comprehensible approach that can easily be implemented in clinical workflow. Of course, the compensation approach needs to be externally validated in future studies,” she said.
Novel Tube Shunt for Refractory Glaucoma
There are various indications for glaucoma drainage implants, including failed trabeculectomy, uveitic glaucoma, neovascular glaucoma, trauma and aphakic glaucoma. However, current commercially available implants have several issues, noted Dr. Victor Koh from Singapore. “In the long run, intraocular pressure control is an issue due to the encapsulation of the conjunctiva over the plate. There can also be complications such as hypotony and shallow anterior chambers, hypertensive phase, tube exposure/conjunctival erosion and cornea decompensation,” he said.
The Paul Glaucoma Implant (PGI), with its micro-sized tube, maximum effective surface area and flexible plate, may just be the solution to the issues listed above.
According to Dr. Koh, compared to commonly used implants like the Ahmed Glaucoma Valve and Baerveldt, the PGI has a bigger plate size, which is able to reduce encapsulation. In terms of wingspan, it is also smaller and more flexible, making it easier to implant. In addition, its smaller outer diameter tube size poses less risk of tube erosion and cornea touch, while its smaller internal diameter tube size helps to prevent hypotony.
* Ehlers JP, Modi YS, Pecen PE, et al. The DISCOVER Study 3-Year Results: Feasibility and Usefulness of Microscope-Integrated Intraoperative OCT during Ophthalmic Surgery. Ophthalmology. 2018 ;125(7):1014-1027.
Editor’s Note: The 5th AOS Congress was held virtually on March 26-27, 2022. Reporting for this story took place during the event.