As recommended by the Clinical Director at Heidelberg Engineering, Christopher Mody
Geographic atrophy (GA), the advanced non-neovascular form of age-related macular degeneration (AMD), represents a growing challenge in ophthalmic care, with an estimated global prevalence of 5 million cases worldwide.¹ As life expectancy rises, so does the impact of GA on patient independence and healthcare systems, but with advancing treatment options and cutting-edge diagnostic technology, eye care professionals are better equipped than ever to manage the condition.²

Heidelberg Engineering aims to deliver imaging solutions that empower clinicians to diagnose, monitor and manage GA with clarity and confidence. The SPECTRALIS® platform, with its multimodal imaging capabilities, plays a central role in enabling high-precision diagnostics and guiding personalized treatment strategies.
From observation to intervention: A new era in GA care
Historically, clinical management of GA was limited to observation. However, two FDA approved intravitreal therapies — pegcetacoplan (Syfovre) and avacincaptad pegol (Izervay) — have demonstrated efficacy in slowing lesion growth by 17-35%, depending on dosing regimen and treatment duration.³⁴ These therapies do not reverse existing atrophy but represent a major step forward in slowing progression and preserving functional vision.
The power of multimodal imaging: Confident diagnostic decisions
Multimodal imaging is critical for identifying GA candidates that are likely to benefit from treatment. The SPECTRALIS imaging platform offers a comprehensive suite of imaging modalities essential for early detection, precise staging and ongoing management of GA. Each imaging technique offers a different insight into a particular aspect of retinal pathophysiology, by reflecting the health of a certain component of the retinal tissue.⁵
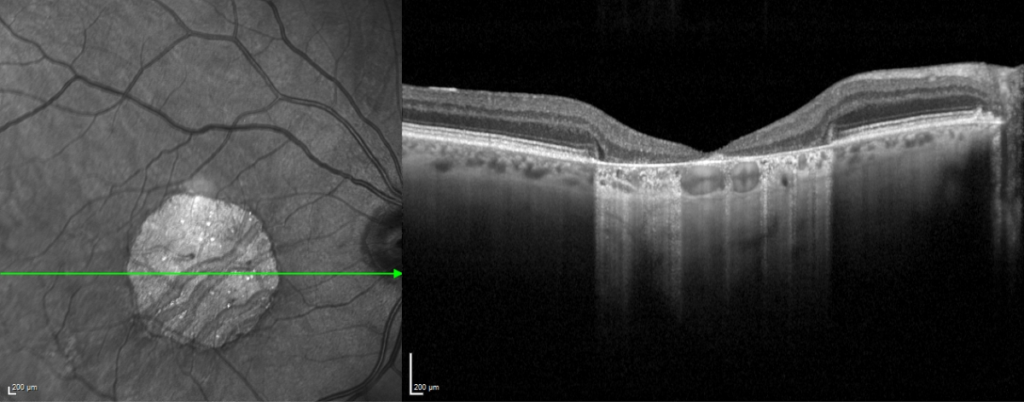
Spectral-Domain OCT (SD-OCT) technology provides high-resolution cross-sectional views of the retina. High-quality SPECTRALIS OCT images allow clinicians to identify pre-atrophic biomarkers such as ellipsoid zone (EZ) disruption, outer nuclear layer (ONL) thinning and choroidal hypertransmission. These features are key to applying CAM (Classification of Atrophy Meeting) definitions for incomplete (iRORA) and complete RPE and outer retinal atrophy (cRORA).⁶
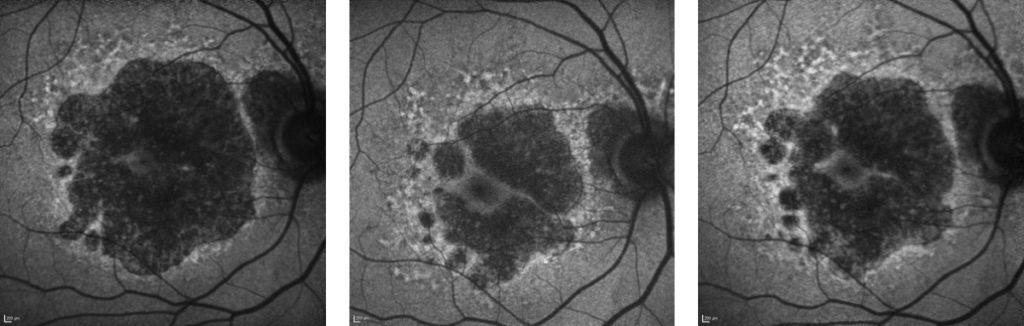
Blue fundus autofluorescence (FAF) has been well-established for many years as a fast, easily repeatable and non-invasive measure for evaluating the pattern and distribution of lipofuscin in the retina.⁷⁸ The SPECTRALIS BluePeak Module enables clinicians to visualize the size and potential for progression of GA lesions.

Near-infrared reflectance (NIR) and en-face OCT imaging offers additional insights, particularly in cases where FAF may be limited by media opacities or foveal pigmentation.⁹ The SPECTRALIS MultiColor Module and Widefield Imaging Module further expand the diagnostic perspective, enabling full visualization of atrophic changes across the macula and beyond. A combined multimodal imaging strategy — using an imaging platform such as SPECTRALIS — is recommended for a comprehensive view and confident treatment planning.⁶
Sign-up and stay tuned for GA: In Focus
Uncover more about GA classification, lesion patterns, risk factors for onset and progression, imaging protocols and the role of AI in GA management.
Click here: www.he-newsletter.com
The role of artificial intelligence in GA analysis

Complementing the multimodal imaging strategy are a host of artificial intelligence (AI) tools that can be integrated into clinical practice that assist the clinician with insights such as automated layer segmentation, quantifying atrophy and photoreceptor loss, and stratifying patients as slow or fast progressors. However, effective use of AI requires high-quality OCT data, standardized scan patterns and compatible infrastructure. Solutions exist, such as HEYEX 2 with Heidelberg AppWay, which makes it easy to seamlessly integrate third-party AI-driven ophthalmic clinical and research applications securely into the existing clinical routine.
Preparing for the future: Clinical recommendations
Advancements, including the first FDA-approved therapies and the development of AI-driven diagnostic tools, offer new hope for managing GA. Eye care professionals can prepare to take advantage of these advancements right away:
- Implement routine imaging protocols for patients with intermediate AMD and GA
- Use fundus autofluorescence and OCT to document lesion extent, monitor progression and identify high-risk phenotypes
- Stay current with internationally accepted terminology and classifications
- Evaluate clinical systems for AI compatibility and standardized imaging outputs
- Engage patients in informed discussions about treatment expectations and disease trajectory
Shaping tomorrow’s vision care today
As therapeutic and technological advances converge, eye care professionals are uniquely positioned to deliver earlier, more targeted interventions that can meaningfully delay vision loss in patients with GA. Heidelberg Engineering is here to support this evolution and unlock the full potential of retinal diagnostics through the expandable SPECTRALIS multimodal imaging platform and AI-enabled innovations via HEYEX 2 with Heidelberg AppWay.
Want to dive deeper into the future of GA diagnosis and management?
This summary highlights key insights from a comprehensive article to be released by Heidelberg Engineering later in 2025.
Subscribe to the Heidelberg Engineering newsletter to be among the first to access the full article and stay informed about the latest advances in retinal imaging and AI-powered eye care.
References
- Wong WL, Su X, Li X, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health. 2014;2(2):e106-16.
- Patel PJ, Ziemssen F, Ng E, et al. Burden of Illness in Geographic Atrophy: A Study of Vision-Related Quality of Life and Health Care Resource Use. Clin Ophthalmol. 2020;14:15-28.
- Heier JS, Lad EM, Holz FG, et al; OAKS and DERBY study investigators. Pegcetacoplan for the treatment of geographic atrophy secondary to age-related macular degeneration (OAKS and DERBY): two multicentre, randomised, double-masked, sham-controlled, phase 3 trials. Lancet. 2023;402(10411):1434-1448.
- Khanani AM, Patel SS, Staurenghi G, et al; GATHER2 trial investigators. Efficacy and safety of avacincaptad pegol in patients with geographic atrophy (GATHER2): 12-month results from a randomised, double-masked, phase 3 trial. Lancet. 2023;402(10411):1449-1458.
- Crincoli E, De Rosa I, Miere A, Colantuono D, Mehanna CJ, Souied EH. Comparison of Multimodal Imaging for the Characterization of Geographic Atrophy. Transl Vis Sci Technol. 2022;11(11):21.
- Sadda SR, Guymer R, Holz FG, et al. Consensus Definition for Atrophy Associated with Age-Related Macular Degeneration on OCT: Classification of Atrophy Report 3. Ophthalmology. 2018;125(4):537-548. [Erratum in: Ophthalmology. 2019;126(1):177]
- Schmitz-Valckenberg S, Brinkmann CK, Alten F, et al. Semiautomated image processing method for identification and quantification of geographic atrophy in age-related macular degeneration. Invest Ophthalmol Vis Sci. 2011;52(10):7640-7646.
- Hwang JC, Chan JW, Chang S, Smith RT. Predictive value of fundus autofluorescence for development of geographic atrophy in age-related macular degeneration. Invest Ophthalmol Vis Sci. 2006;47(6):2655-2661.
- Corvi F, Corradetti G, Laiginhas R, Liu J, Gregori G, Rosenfeld PJ, Sadda SR. Comparison between B-Scan and En Face Images for Incomplete and Complete Retinal Pigment Epithelium and Outer Retinal Atrophy. Ophthalmol Retina. 2023;7(11):999-1009.