Luminaries from across the Asian vitreoretinal ophthalmology community gathered to celebrate the beginning of the 17th Congress of the Asia-Pacific Vitreo-retina Society (APVRS 2024)—and hear about the latest in neovascular age-related macular degeneration, geographic atrophy and diabetic retinopathy.
APVRS 2024 Singapore has officially kicked off, as doctors and industry from across Asia and the world descend on Singapore for another edition of the region’s annual retina fiesta.
Congress President Prof. Gemmy Cheung (Singapore) delivered the opening address, where she led off by thanking the APVRS Secretariat and the over 2,000 participants representing more than 40 countries in attendance.
In her speech, Prof. Cheung touched on the Congress’ theme—and why it’s so critical in the context of today’s modern vitreoretinal landscape.
“The landscape of healthcare constantly changes and faces challenges. Population aging and modern lifestyles have had major impacts on eye and retinal health,” she said, citing the rise of diseases like age-related macular degeneration (AMD), diabetic retinopathy (DR) and pathologic myopia. “With this in mind, the theme of this year’s Congress was selected as ‘Transforming Retinal Disease Management With Technology.’”
APVRS President Prof. Hiroko Terasaki (Japan) echoed these sentiments, urging delegates to make use of the Congress as a launchpad for collaborative innovation. “This is not just an event, it’s a unique opportunity for us to connect, to learn from one another—and to drive innovation in the field,” she said.
Tano Lecture spotlights anti-VEGF alternatives in ocular angiogenesis
After a live performance from Singaporean sand artist and light painter Lawrence Koh, which featured the artist creating a series of images depicting the city and its cultural and ophthalmic heritage, the first of the session’s three marquee award presentations began with the APVRS Tano Lecture.
This year’s honoree, Asian ophthalmology titan Prof. Dennis Lam (Hong Kong), spoke about the current drug approval process in the region and potentially exciting new candidates in development for neovascular AMD (nAMD) and DR.
The first de novo agent he discussed was the small molecule tubulin polymerization inhibitor (TPI) KX-02 for nAMD. Derived from a treatment for precancerous skin lesions, Prof. Lam described KX-02’s two main advantages. The first, he said, lies in the increased absorption potential it has compared to large-molecule anti-VEGF agents that represent the current standard of care. The second is that KX-02 injections could potentially be peribulbar.
The second drug he described is DR candidate biologic pegylated (PEG)-arginase, a non-essential amino with neovascularization-suppressive, angiogenic-reparative and neuroprotective potential.
According to Prof. Lam, one of the key drivers of excitement around the drug is a second generation, called PA-02, which has increased the agent’s half-life and decreased the number of isomers from 6-8 to just 1.
In the end, Prof. Lam believes these two drugs and their differentiated mechanisms of action from current standard-of-care anti-VEGF have great potential—whether used in concert with anti-VEGF agents or as standalone treatments.
“Anti-VEGF may not be the only choice in the future for these diseases,” he concluded.
The unequal global fight against DR
World-renowned retinal specialist Prof. Sobha Sivaprasad (United Kingdom) took the stage next to deliver the APVRS International Award Lecture. In keeping with the spirit of the award, Prof. Sivaprasad used her turn at the podium to explore global disparities in DR management.
Diabetes is on the rise around the globe, Prof. Sivaprasaid said, and this rise is not uniform. Three out of four persons with diabetes live in low- and middle-income countries, she said, holding up outliers in south Asia like Bangladesh (highest rates of DR), India (highest absolute numbers), Afghanistan (highest proportion of undiagnosed diabetes) and Pakistan (highest diabetes rate).1
“All four of these countries have inadequate public health systems, and the patients in these countries have to rely on out-of-pocket expenditure for their health,” she said. “These disparities in South Asia apply throughout the world, especially in low- and middle-income countries.”
Despite this, however, the majority of DR research has taken place mostly in white, high-income countries, leaving much to be desired for solving region- and ethnicity-specific problems in DR—especially with minority ethnic groups exhibiting a higher risk of developing DR and vision-threatening (VT) DR.
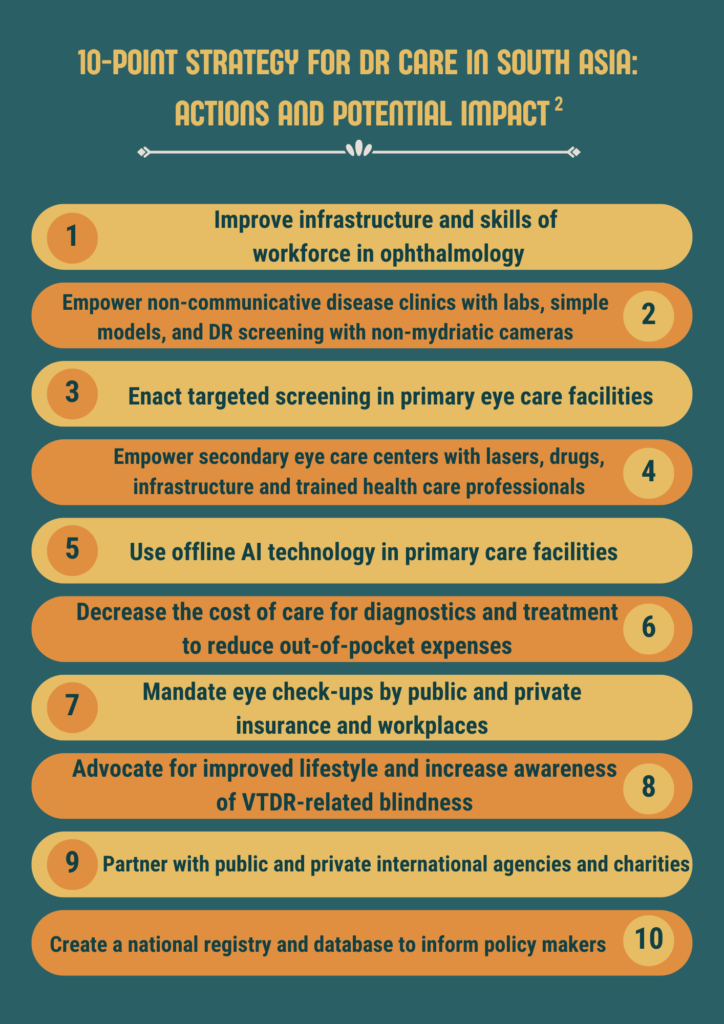
So what’s the solution? Prof. Sivaprasad on potential new low-resource screening solutions, including predictive risk models and offline AI-enabled screening fundus cameras and agents like fenofibrate for reducing progression risk, Prof. Sivaprasad showed a recently published ten-point plan that could save sight worldwide.2
There is, however, one caveat that she expressed before concluding. “We have done a lot of work in the last five years to start to see the end of vision-threatening diabetic retinopathy, but there is a lot more to be done.”
Geographic atrophy endpoint mismatch mayhem
Geographic atrophy (GA) and the efficacy of complement inhibition have dominated ophthalmic conferences around the world of late. At the heart of the matter is the seeming discord between structural and functional endpoints in clinical trials, with many Phase III trials showing reductions in GA growth without an alteration in the rate of vision loss.
Awardee Prof. Usha Chakravarthy (United Kingdom) dedicated her College of Ophthalmology to the topic, and in the process shed new light on one of the vitreoretinal subspecialty’s great debates.
The first piece to the puzzle for Prof. Chakravarthy is the variability of GA growth rates in individual patients—and especially the phenotype (lesion location, focality, autofluorescence phenotype and pseudodrusen).
Another key point is that there are many measures of vision, from best-corrected and low-luminance visual acuity to reading rates, microperimetry and more. These measures of vision, according to Prof. Chakravarthy, worsen at different rates, causing problems in assessing actual functional loss.
So how can scientists choose better endpoints that correlate structural findings with function–and identify patients that will benefit from the current lineup of complement inhibitors?
“By combining growth rate information with focal features and phenotype of the GA lesion, I can identify subgroups that are at risk of losing BCVA,” Prof. Chakravarthy said.
“For these patients, microperimetry and looking at scotomatous endpoints—and particularly mapping visual function in the center of the eye—correlates best with BCVA,” she said, “and working with categorical trial endpoints as outcomes is an alternative to assessing linear changes and identify subgroups that may benefit from interventions.”
Editor’s Note: Reporting for this story took place during the 17th Congress of the Asia-Pacific Vitreo-retina Society (APVRS 2024) from 22-24 November in Singapore.
References
- IDF Diabetes Atlas. Available at https://diabetesatlas.org/. Accessed on 22 November 2024.
- Das T, Islam K, Dorji P, et al. Health transition and eye care policy planning for people with diabetic retinopathy in south Asia. Lancet Reg Health Southeast Asia. 2024;27:100435.



