Telemedicine strategies represent a booming trend in the delivery of effective eye care to underserved regions around the globe. The associated technology has allowed for an evolution of telemedicine applications from research to clinical use, most often addressing screening challenges and access to an expert referral. In eye care, teleophthalmology targets either diseases for which there is lack of available expertise, such as retinopathy of prematurity, or diseases that cause overwhelming burden, such as diabetic retinopathy or glaucoma.
Within peer-reviewed literature, there are hundreds of publications referencing teleophthalmology approaches. The most common approach is the “store-and-forward” method, where digital images are taken and then forwarded for interpretation and appropriate follow-up.
In addition, real-time examinations are starting to take place digitally. These are great steps forward in patient diagnostics, but there can be specialist accessibility issues. For example: What can be done if a patient’s required treatment is identified, but they are far away from any specialist that can deliver it? Addressing this “now what?” challenge would typically spiral into a flurry of expedited logistics and funding requests to transport the patient to the specialist or surgeon.
But what if the equipment was in place for the patient to be effectively treated at their local facility, and then linked to the specialty care? Is teleophthalmology treatment feasible? Dr. Igor Kozak, a clinical lead at the Moorfields Eye Hospital Centre in Abu Dhabi, and his colleagues believe it is thanks to the concept of retinal telephotocoagulation. They have taken the concept of teleophthalmology beyond the scope of a diagnostic screening tool, and applied it to the actual treatment of patients with diabetic macular edema (DME).
This is a critical study – an estimated 285 million people have diabetes mellitus worldwide and approximately 31 million have vision-threatening diabetic retinopathy, including DME. The study by Kozak et al., recently published in Graefe’s Archives of Clinical and Experimental Ophthalmology, introduces the idea that actual treatments can be performed between or among distant clinical sites.
“This, for the first time, moves teleophthalmology up to therapeutic level. It utilizes the concept of image transfer and alignment, along with retinal laser photocoagulation, using navigation and eye tracking. With this concept, clinical sites can exchange pre-programmed treatment plans which can be applied to patients at any location,” explained Dr. Kozak.
The authors stress that there are two essential components of successful retinal telephotocoagulation: image registration and transfer. Image registration is the transformation of images acquired at different time points, or with different imaging modalities, into the same coordinate system. This allows the images to be combined, while maintaining important structural and functional details. A minimum of three corresponding landmarks must be identified by the operator in both images to calculate a multidimensional transformation matrix for registration.
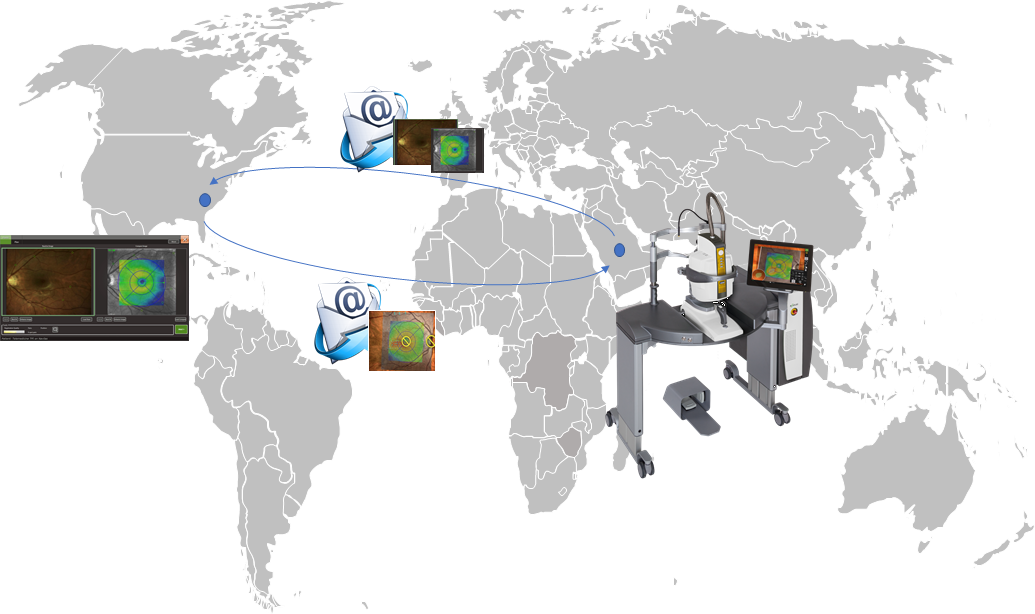
The study involved 16 eyes of 10 subjects diagnosed with DME, that underwent navigated focal laser photocoagulation using their novel teleretinal treatment plan. At King Khaled Eye Specialist Hospital in Riyadh, Saudi Arabia, patients underwent retinal imaging and fundus fluorescein angiography, which were registered using the NAVILAS Contact registration software (NAVILAS®, OD-OS Inc. Berlin, Germany). The images were then transmitted to a second clinic in an encrypted format.
At the second clinic, Palmetto Retina Center in West Columbia, South Carolina, USA, retina specialist and co-investigator, Dr. John Payne, created image-based treatment plans from the original imaging, targeting leaking microaneurysms and placement of computerized grid patterns in areas of diffuse leakage. The treatment plans were then transmitted back-to-back to King Khaled Eye Specialist Hospital where the macular laser photocoagulation was performed, using the same NAVILAS system.
Investigators looked at the feasibility of image transfer and performing navigated laser photocoagulation for subjects at two distinct clinics. Additionally, the patients’ eyes were followed for three months after treatment, to assess changes in best-corrected visual acuity (BCVA) and central retinal thickness (CRT) by spectral-domain optical coherence tomography.
Kozak and colleagues were able to successfully execute the treatment plan in all 16 eyes. No adverse events occurred and all eyes demonstrated improvement in the area of retinal edema: BCVA remained stable and CRT improved from 290.1 ± 37.6 μm at baseline to 270.8 ± 27.7 μm (p = 0.005) after three months.
This has been the first study to apply a therapeutic teleophthalmology approach, rather than strictly diagnostic. It demonstrates safety and feasibility of telephotocoagulation to perform navigated retinal laser treatments, regardless of geographical distance.
This novel concept has the potential to open a new chapter in ophthalmic care, as described by Dr. Kozak, “This can be executed online or as a step-wise process. Furthermore, it provides ability to standardize retinal laser treatments at multiple sites for the purpose of clinical trials research as well as improving access and enhancing patient care.”
This standardization could address inter-operator variability in conventional laser photocoagulation, which could potentially impact comparison to other treatments. Additionally, the concept of retinal tele-navigation could be applied to vitreoretinal and robotic surgical procedures guided by image-based navigation.
Reference:
Kozak I, Payne JF, Schatz P, et al. Teleophthalmology image-based navigated retinal laser therapy for diabetic macular edema: a concept of retinal telephotocoagulation. Graefes Arch Clin Exp Ophthalmol. 2017 [Epub ahead of print].