nAMD care is evolving fast, with durable drugs, sci-fi gene therapy, virtual clinics and more.
Day 1 of the 25th Congress of the European Society of Retina Specialists (EURETINA 2025) wasted no time diving into the deep end. The afternoon symposium on neovascular age-related macular degeneration (nAMD) felt less like a refresher course and more like a forward-facing masterclass: equal parts science, strategy and a glimpse of the not-so-distant future.
From molecular culprits of vision loss to gene therapies that sound lifted from a sci-fi script (but aren’t), the session mapped where we stand and where we’re headed. And yes, there were plenty of take-home pearls along the way.
Understanding the mechanisms of nAMD vision loss
Prof. Usha Chakravarthy (UK) opened the session with fresh insights into macular atrophy and fibrosis in nAMD, noting how these complications drive severe vision loss even in the era of anti-VEGF therapy.
“In chronic neovascular AMD, we always see atrophy and fibrosis, and we know from data from many years ago that these are associated with severe vision loss,” Prof. Chakravarthy explained. “It doesn’t matter how you look at visual function—distance vision, near vision, contrast—all these are lower in eyes that have either atrophy or fibrosis or both.”
READ MORE: GLP-1 Agonists Associated with Doubled Risk of Neovascular AMD, Study Finds
Drawing on seven-year IVAN trial data, she showed how persistent hyperreflective material (HRM) on optical coherence tomography (OCT) is a strong surrogate for fibrosis. When HRM replaces the outer retina, visual function plummets by about 30 letters.1
The AVENUE trial added more nuance, revealing four distinct HRM evolution patterns after anti-VEGF treatment. Outcomes were best when HRM either resolved entirely or developed a clear boundary with the neurosensory retina.2
“Complete resolution or development of a boundary internal to the hyperreflective material is associated with better function and lower macular atrophy risk,” Prof. Chakravarthy concluded.
Distinguishing exudative from non-exudative OCT findings
Dr. Rosa Dolz-Marco (Spain) tackled one of the trickiest diagnostic challenges: telling true exudation apart from its look-alikes.
“It’s important to recognize these features, know their characteristics and differentiate them from real fluid in order to avoid overtreatment,” she stressed.
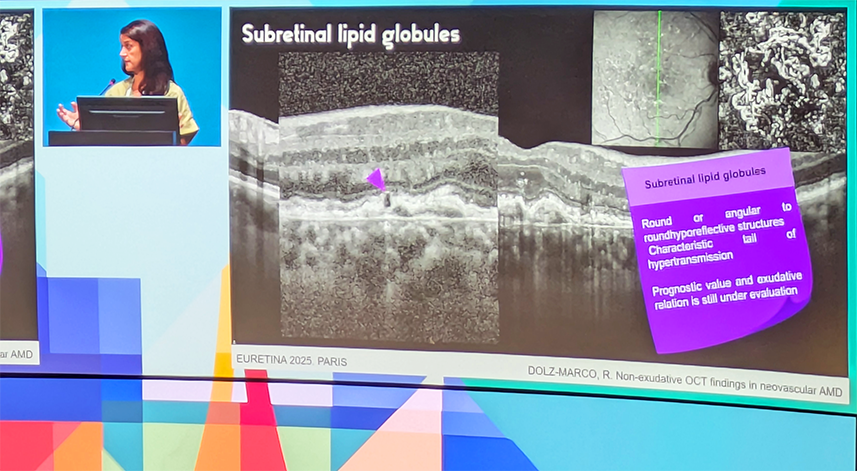
She outlined several common culprits—outer retinal tubulation, pseudocysts and subretinal lipid globules—that can masquerade as fluid. Pseudocysts, she noted, often appear in areas of thin or normal-thickness retina, while real exudation typically produces thickening.
Dr. Dolz-Marco also drew attention to the differences between the double-layer sign, often drusen-like and homogenous, and the thicker, multilayered appearance more suggestive of macular neovascularization.
Next-generation anti-VEGF therapies
Prof. Dr. Sandrine Zweifel (Switzerland) highlighted the clinical impact of extended durability agents: faricimab (approved January 2022) and high-dose aflibercept (approved August 2023).
“So far more than eight million vials of faricimab and more than 2.7 million vials of high-dose aflibercept have been distributed,” she reported, underscoring their rapid uptake.
READ MORE: Bayer Notches Dual EYLEA 8mg Wins With China nAMD Approval and EU 6-Month Interval Extension
Real-world outcomes from the Swiss Retina Research Network showed that in treatment-naive patients, faricimab delivered both functional and anatomical gains over 12 months. In switch patients, a 325-patient study published in Ophthalmology Retina found stable vision with extended treatment intervals.3
Similarly, early real-world results with high-dose aflibercept suggest patients can maintain outcomes with longer dosing intervals compared to the standard formulation, though with less follow-up time.4
“We can achieve longer treatment intervals. This, of course, leads to reduced GP burden. We have a high safety profile,” Dr. Zweifel concluded, while cautioning that fibrosis and macular atrophy remain stubborn challenges.
READ MORE: The Potential for Better and Faster Drying with Longer Treatment Intervals
From science fiction to reality
Looking further ahead, Prof. Arshad Khanani (USA) charted the accelerating progress of gene therapy for nAMD.
“It’s an evolving field and it’s going to be a reality in the next few years, whether you like it or not,” he stated. “I was here last year giving the same talk and only one program was in Phase III, and now we have three in Phase III.”
The three programs include:
- Sura-vec (formerly ABBV-RGS-314; REGENXBIO, Maryland, USA), a subretinal anti-VEGF transgene delivery approach
- Ixoberogene soroparvovec (Adverum Biotechnologies, California, USA), an intravitreal therapy using a directed evolution vector
- 4D-150 (4D Molecular Therapeutics, California, USA), an intravitreal dual-transgene therapy targeting VEGF-A and VEGF-C
According to Prof. Khanani, data show 50% to 60% of patients remain injection-free after a single treatment, with others seeing 70% to 90% reductions in treatment burden. In newly diagnosed patients, injection-free rates reach 80%, with a 94% reduction in treatment need compared to standard therapy.
“We have seen long-term maintenance or improvement in visual acuity with CST [central subfield thickness] control with 57% injection-free and a significant reduction in treatment burden for these patients,” Prof. Khanani said of the 4D-150 program.
“It’s very exciting that it’s not science fiction anymore. It’s actually a reality,” he concluded.
READ MORE: Exegenesis Bio Provides Updates on nAMD Gene Therapies
Transforming AMD care delivery
Prof. Pearse Keane (UK) closed the session with a look at how telemedicine is reshaping AMD services at Moorfields Eye Hospital.
“Ophthalmology has overtaken orthopedics as the number one busiest specialty in the National Health Service in terms of clinic appointments,” he noted, emphasizing the need for fresh solutions.
Moorfields is deploying four models:
- Video consultations, particularly for emergency triage
- Hospital-based virtual clinics, where imaging is acquired on-site and read remotely
- Home monitoring via smartphone apps and printable visual acuity (VA) charts
- Community diagnostic hubs, including clinics set up in shopping centers
The impact has been dramatic. Before the pandemic, 80% of retina appointments were in-person. Now, half are virtual. According to Prof. Keane, Moorfields currently manages more than 1,000 virtual visits per week.
Looking to the future, he envisions a workflow where data from any location can feed into automated analysis, with AI-powered assistants increasingly supporting patient interaction.
READ MORE: New Study Demonstrates AI’s Reliability in Home OCT Analysis for nAMD
If the symposium proved anything, it’s that nAMD care is evolving at breakneck speed. Between durable anti-VEGF treatments, gene therapy programs edging toward prime time and telemedicine models reshaping service delivery, the future is already knocking.
Fibrosis and macular atrophy remain the tough nuts to crack, but after a day like this, one can’t help but think that even those problems may not stay unsolved forever.
Catch all the latest stories, sessions and daily insights on our EURETINA coverage page.
Editor’s Note: The 25th EURETINA Congress is being held from 4-7 September, in Paris, France. Reporting for this story took place during the event. This content is intended exclusively for healthcare professionals. It is not intended for the general public. Products or therapies discussed may not be registered or approved in all jurisdictions, including Singapore.
References
- Chakravarthy U. Characterization of associations between macular atrophy and subretinal fibrosis in treated neovascular AMD: 7 year findings from the IVAN trial. Inv Ophthalmol Vis Sci. 2022;63(7):1322.
- Yu S, Bachmeier I, Chakravarthy U, et al. Hyperreflective material boundary remodeling in neovascular age-related macular degeneration: A post hoc analysis of the AVENUE trial. Ophthalmol Retina. 2023;7(11):990-998.
- Grimaldi G, Ambresin A, Zweifel S, et al. One-year outcomes after switching to faricimab in eyes with pretreated neovascular age-related macular degeneration: A Swiss Retina Research Network Report. Ophthalmol Retina. 2025:S2468-6530(25)00124-1.
- Palm C, Zweifel SA, Gabathuler F, Cozzi M, Fasler K. Efficacy of aflibercept 8 mg in pretreated age-related macular degeneration. J Clin Med. 2025;14(1):4900.
