Italian vitreoretinal surgeon Dr. Barbara Parolini presented a new staging system and guidelines for the management for myopic traction maculopathy (MTM) during the LV Prasad Eye Institute (LVPEI) Vitreoretinal Surgery Masterclass 2022 webinar.
Pathogenesis of MTM
Myopic traction maculopathy (MTM) is a complex disease affecting approximately 30% of eyes with pathologic myopia. Its pathologic features may also include lamellar or full thickness macular holes (FTMH), shallow foveal detachments and inner retinal fluid.
“In a normal situation, there is the centripetal force that points to the fovea and keeps the retina together. This force is due to the combination of neural cells, external limiting membrane and internal limiting membrane. In MTM, various centrifugal forces play against this centripetal force. The forces perpendicular to the retina induce schisis and detachment; while the forces tangential to the retina induce foveal splitting,” said Dr. Barbara Parolini.
She further explained that the centrifugal force from the posterior eyewall elongates the eye posteriorly and detaches the sclera from the retina. Meanwhile, the centrifugal force from the lateral eyewall enlarges the eye and induces detachment in the lateral part of the eye. Centrifugal force from the vitreous pulls the retina anteriorly, and centrifugal force from the interface (tangential to the retina) leads to FTMH.
“The forces can also be combined. You can have centrifugal perpendicular force (from the eyewall and vitreous) and centrifugal tangential force (from eyewall and vitreous) and you will end up with a macular detachment combined with macular hole,” she noted.
The MTM Staging System
To improve the diagnosis and management of MTM, Dr. Parolini and her colleagues published the MTM Staging System (MSS), which is a comprehensive description of OCT-based classification of MTM.*
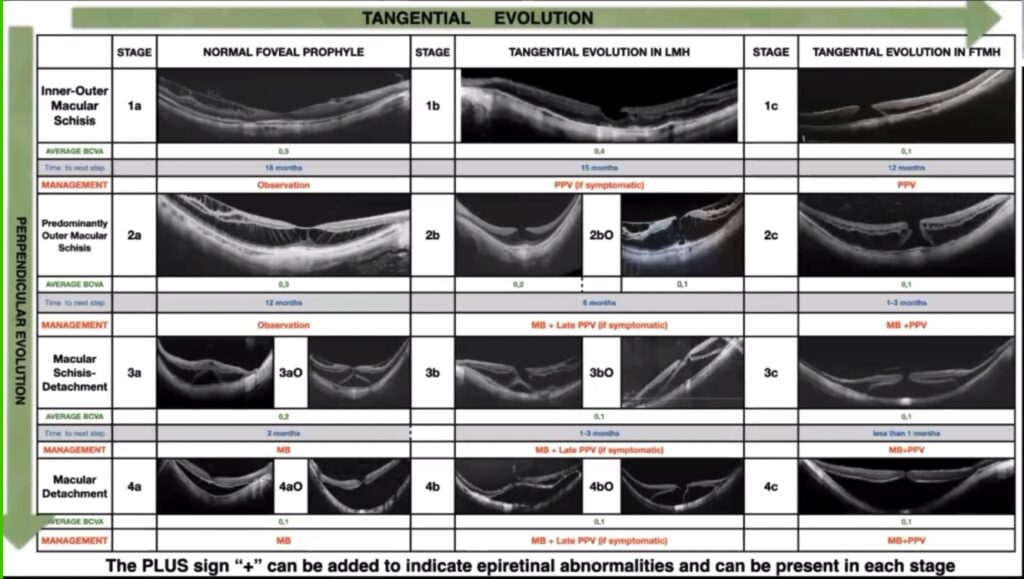
“The study of the natural history of MTM demonstrated that MTM is divided not in types but in stages. Stage 1 refers to inner-outer macular schisis, stage 2 is predominantly outer macular schisis, stage 3 is macular schisis and detachment and stage 4 is complete macular detachment without schisis because the inner forces are released. Within these four stages, there are three stages of the fovea — stage a: normal foveal profile, stage b: tangential evolution in lamellar macular hole (LMH) and stage c: tangential evolution in FTMH,” Dr. Parolini explained.
She noted that the MSS serves as a base for definitions and prognosis, as well as a guideline to treatment.
“If you have a patient in stages 1a and 2a, I advise you not to do anything because the evolution is very slow and visual acuity is good. You can ask the patient to come back in 12-18 months. For stage 1b and 1c, I advise vitrectomy but for 1b, only if vision is declining. For stage 3a and 4a, just do macular buckling. Do not touch the retina from the inside. For stage 2b, 3b and 4b, I advise to apply macular buckle and add vitrectomy as the second step only if the lamellar hole remains symptomatic. For stage 2c, 3c and 4c, I advise to perform macular buckling and pars plana vitrectomy (PPV).
“In summary, retinal pattern, such as schisis and detachment, should be solved by a macular buckling because perpendicular forces should be pushed. While foveal pattern (holes) should be solved by PPV, as tangential forces should be peeled,” she said.
She further explained that when there is a centrifugal force detaching the scleral from the retina, the way is to push the scleral to the retina with the macular buckle. Meanwhile, if there is a macular hole, it should be treated with vitrectomy and internal limiting membrane (ILM) peeling. When combined forces are present, treatments should be combined as well.
Inserting the Macular Buckle
The macular buckle is a device made to shorten the axial length at the posterior pole.
“If you are using just the macular buckle, I advise starting with paracentesis to lower the intraocular pressure. The easiest quadrant to insert the macular buckle is the superotemporal quadrant, where you can easily reach the fovea since there are no oblique muscles,” Dr. Parolini suggested.
“Use the panoramic viewing system to locate the buckle. Centration is a key factor in this type of surgery. Sutures can be applied anteriorly close to either the lateral rectus muscle or superior rectus muscle. You can use one or two sutures to fixate the buckle and avoid tilting.”

She showed a case of MTM with stage 4c detachment and full-thickness macular hole, and the patient’s vision was counting fingers. “If you do a vitrectomy with such a huge staphyloma, you will have a good chance to attach the retina under gas and keep the hole open, but when the gas is removed, there’s a high chance that the retina will re-detach. Putting in silicone oil can attach the retina, but when the oil is removed, the retina will re-detach. On the other hand, the application of a macular buckle with vitrectomy gas and ILM peeling can achieve an attached retina, a hole that is closed, and an increase in visual acuity,” she said.
“My suggestion is to follow the MSS classification system and guidelines of treatment. Choose the model of buckle you prefer, and help me validate the MSS,” she concluded.
*Parolini B, Palmieri M, Finzi A, Besozzi G, Lucente A, Nava U, Pinackatt S, Adelman R, Frisina R. The new Myopic Traction Maculopathy Staging System. Eur J Ophthalmol. 2021;31(3):1299-1312.
Editor’s Note: The LV Prasad Eye Institute’s Vitreoretinal Surgery Master Class, aptly titled “Tough case or a surgical surprise, let’s learn the enterprise” was held from February 26 to 27, 2022.



