Can VR make vision tests easier, or chatbots lighten clinic load? EURETINA 2025 offered bold answers.
The second day of the 25th Congress of the European Society of Retina Specialists (EURETINA 2025) put artificial intelligence not just under the microscope, but squarely in the hands of clinicians. In a buzzing session hall at the Palais des Congrès, AI was tested, debated and demystified.
With Prof. Dr. Martin Zinkernagel (Switzerland) and Prof. Pearse Keane (UK) chairing, the session sprinted from clinic letters to chatbots VR perimetry and intraoperative OCT, before closing on equity metrics that could change regulation itself.
Large language models
Large language models (LLMs) have become part of everyday life, but their clinical potential is only just being realized. Moorfields Eye Hospital’s Dr. Ariel Ong (United Kingdom) argued that the true promise lies in turning the “narrative chaos” of healthcare into structured insights.
Only a fraction of healthcare data exists in structured fields; most is trapped in clinic letters, referral notes and reports. Traditional natural language processing (NLP) required immense effort and often failed when faced with new documentation styles. By contrast, Dr. Ong explained, “LLMs can generalize to many tasks with little to no labeling and capture clinical context that’s more subtle.”
READ MORE: AI Tools in Ophthalmology: From Virtual Scribes to Surgical Planning
Her team is testing ways to extract meaningful clinical variables from millions of patient letters—unlocking a resource for both care and research. She also pointed to the power of AI in clinical trials, where patient eligibility screening could be accelerated if models can explain their reasoning. As she put it, “The real challenge is not whether these tools can do something, but how—and whether—we adopt them responsibly.”
Dr. Ong’s closing emphasis on co-intelligence was the session’s leitmotif: empower researchers and clinicians, don’t replace them.
Chatbots in retina clinics
While Dr. Ong focused on data extraction, Dr. Fares Antaki (Canada), vitreoretinal surgery fellow at Cleveland Clinic, asked whether chatbots might change the very rhythm of clinical practice. His answer: yes, but as an ally, not a rival.
Dr. Antaki highlighted two areas. First, workflow support: AI scribes listen to consultations, generate notes and produce simple patient summaries. Second, clinical triage: AI assistants are available 24/7 to answer urgent questions and redirect patients appropriately.
One of his most striking ideas was the introduction of ‘vibe coding’, where clinicians build apps without writing code. “You can use English to build software applications,” he said, demonstrating how a specialist could design a triage chatbot in minutes by conversing with an AI agent.
READ MORE: AI Improves AMD Diagnosis Accuracy and Speed. But Can We Trust It?
When asked whether he personally uses AI for medical help, Dr. Antaki didn’t hesitate: “All the time.” He added that, for him, ChatGPT remained the most engaging and effective model. His point was clear—AI is already woven into the clinician’s toolkit, but its safe integration into official systems still requires validation and oversight.
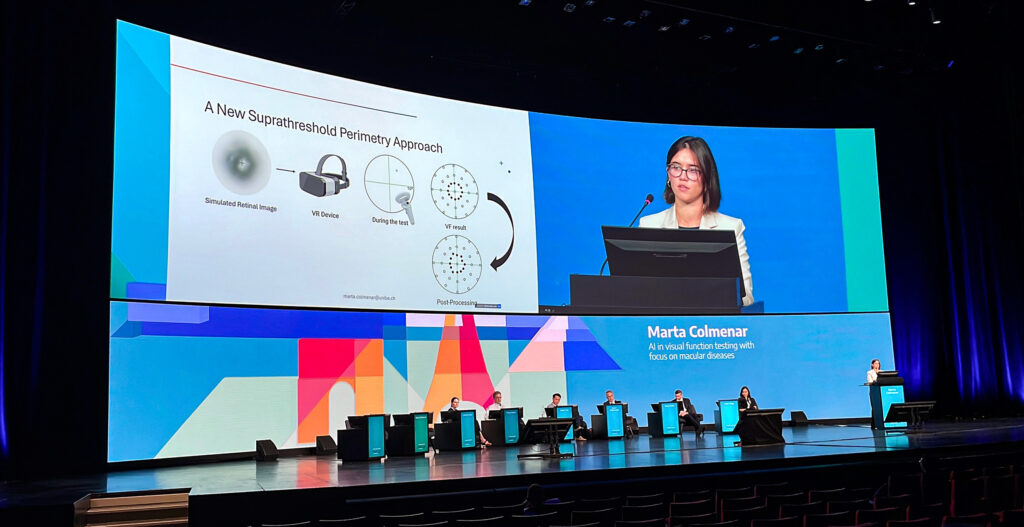
Rethinking vision testing with VR
For patients with advanced macular disease, central fixation is often impossible. So how do you test vision when patients can’t fixate? That’s the problem University of Bern PhD Candidate Marta Colmenar Herrera (Switzerland) tackled with her group’s work on AI-assisted fixation-agnostic perimetry in virtual reality.
Her team built a VR-based, gaze-contingent suprathreshold perimetry for the central 10 degrees, with a large fixation cross for orientation even when the center is missing. “We track gaze continuously and present a stimulus related to the gaze,” she explained, allowing even those with unstable fixation to complete the exam.
Early studies with 26 eyes showed good agreement with standard imaging, and—crucially—patients tolerated the VR headset well. Ms. Colmenar Herrera noted that “most of them were happier doing the virtual reality test than the microperimetry,” even though the average age was around 80.
The roadmap is practical: add thresholding at the atrophy border, seed customized patterns from imaging and keep adapting to the patient rather than forcing the patient to adapt to the test. It’s AI as ergonomics.
READ MORE: New Study Demonstrates AI’s Reliability in Home OCT Analysis for nAMD
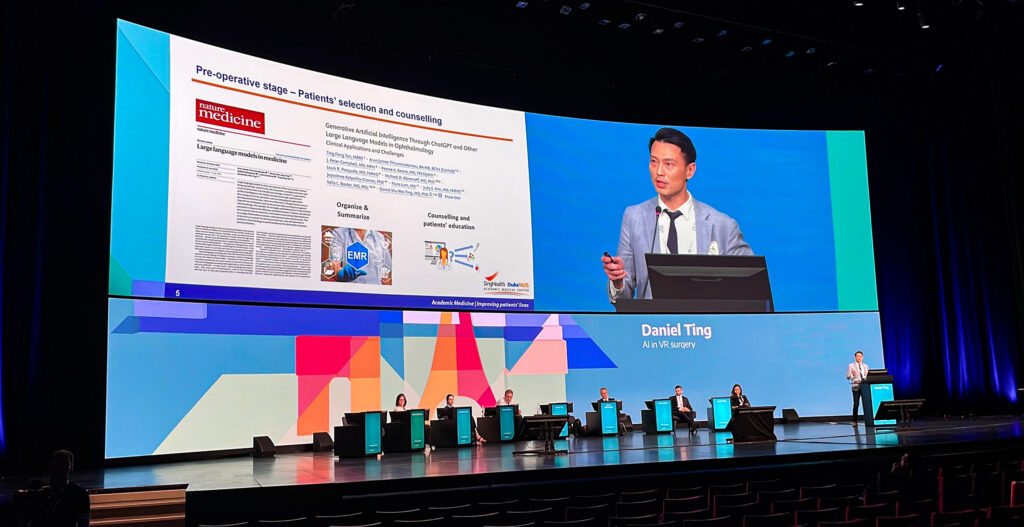
AI’s role in the OR
Moving from clinic to theatre, Prof. Daniel Ting (Singapore) explored how AI is being integrated into vitreoretinal surgery. He broke the workflow into three phases: pre-op, intra-op and post-op.
Preoperatively, LLMs can help summarize complex referral histories or support patient counseling. Imaging algorithms can already detect conditions such as macular holes or retinal detachments. Intraoperatively, Prof. Ting sees major potential in pairing intraoperative OCT (iOCT) with AI segmentation to provide real-time feedback.
“If we could couple iOCT with AI segmentation algorithms to quantify how much gene therapy has already gone into the subretinal space, I think that would be ideal,” he said.
He also pointed to opportunities for automated surgical summaries that could save time after lengthy cases. As for robotics, Prof. Ting acknowledged their promise for tremor reduction and precision but dismissed full autonomy as decades away.
READ MORE: VR Surgery Goes Digital
As for the perennial question—will robots do this on their own? Prof. Ting kept both feet on the ground. The frontier is tremor suppression, precision and safety prompts; full autonomy is far off. “I would be surprised maybe in 50 years… I’m not sure,” he admitted, underlining that augmentation, not replacement, remains the goal.
Ensuring AI sees fairly
The final word came from Prof. Catherine Egan (United Kingdom), who tackled perhaps the most pressing question: Can AI be fair? First, she reminded the audience that bias is not theoretical: “People died because pulse oximeters overestimated blood oxygen levels in people with more pigmented skin.”
In ophthalmology, algorithms for diabetic retinopathy screening are being rolled out globally, but training datasets may not reflect the diversity of patient populations.
READ MORE: Retinal Imaging and AI-Powered Analysis in the Palm of Your Hand
Prof. Egan’s team developed the Retinal Pigment Score (RPS), a continuous, image-derived measure of retinal background pigmentation. “We sought to develop a metric that could describe datasets and be used as a variable to compare diagnostic algorithms,” she explained.
Their findings showed that while overall accuracy was similar across pigmentation levels, false-positive rates varied significantly between algorithms. That means some patients could face unnecessary anxiety or treatment depending on the system used.
Prof. Egan was unequivocal about the implications: “I’d like to see this become a regulatory requirement, and retina could potentially lead the way.” By insisting on transparency and fairness, she argued, ophthalmology can set the standard for other fields.
Human hands on the wheel
If there was one thesis running through the session, it was this: AI is transformative only when it is collaborative. Every speaker underscored the same truth in different ways—these tools work best not as replacements, but as partners. For Dr. Ong, that meant co-intelligence. For Dr. Antaki, it meant allyship in workflow. For Ms. Colmenar Herrera, ergonomics. For Prof. Ting, augmentation. For Dr. Egan, fairness.
The roadmap is clear. Keep humans in the loop. Validate relentlessly. Publish not just accuracy, but equity. Then ship the tools that give clinicians back time, patients back confidence and all of us a cleaner line of sight to better outcomes. AI may be rewriting the script of retina, but as this session showed, the authorship remains firmly human.
Explore the latest retina breakthroughs in our daily EURETINA coverage.
Editor’s Note: The 25th EURETINA Congress is being held from 4-7 September, in Paris, France. Reporting for this story took place during the event. This content is intended exclusively for healthcare professionals. It is not intended for the general public. Products or therapies discussed may not be registered or approved in all jurisdictions, including Singapore.
