A groundbreaking retinal implant study shows that restoring central vision in patients with GA due to AMD may soon move from sci fi to clinical reality.
For years, the possibility of restoring sight for patients suffering from geographic atrophy (GA) due to age-related macular degeneration (AMD) felt like something reserved for futuristic movies, not peer-reviewed journals.
As far as GA is concerned, the first available therapies—pegcetacoplan and avacincaptad pegol—target the complement cascade to slow disease progression. Both treatments, recently approved by the FDA, require intravitreal injections every one to two months.
While these therapies delay the march of GA, no approved treatments, investigational approaches or cell-based therapies have yet demonstrated meaningful visual improvement.1 Today, however, that long-standing limitation may be shifting.
A new study in The New England Journal of Medicine1 evaluating a photovoltaic retina implant microarray (PRIMA) system—a subretinal photovoltaic implant—shows that restoring functional central vision among patients with GA due to AMD is now possible.
READ MORE: Sheets, Chips & Switches: Practical Paths to Vision Restoration
The PRIMAvera study
The PRIMAvera study1 (Restoration of Central Vision With the PRIMA System in Patients With Atrophic AMD) involved 38 participants at 17 clinical sites across five European countries, all with bilateral GA and visual acuity not lower than 1.2 logMAR (20/320) in the study eye.
“The PRIMA system restored central vision and led to a significant improvement in visual acuity from baseline to month 12,” the study’s authors reported.
At 12 months, 32 patients completed follow-up with remarkable results1:
- 26 of 32 participants (81%) had a clinically meaningful improvement in visual acuity (≥0.2 logMAR).
- Using multiple imputation to address the missing data, the estimated rate of clinically meaningful improvement for all participants was 80%.
- The maximum improvement with PRIMA glasses at 12 months reached 1.18 logMAR (59 letters).
“At 12 months, 84% of the participants (27 of 32) could read letters, numbers and words with prosthetic vision at home; 69% (22 of 32) reported medium-to-high user satisfaction with the PRIMA system,” the authors reported.
How does the PRIMA system work?
The system includes two major parts:
- One 2 x 2 mm silicon implant with 378 photovoltaic pixels
- One pair of smart glasses that projects the near-infrared light (880 nm) onto the implant
“The (PRIMA) system is a combination of a subretinal photovoltaic implant and glasses that project near-infrared light to the implant in order to restore sight to areas of central retinal atrophy,” the authors of the study reported.
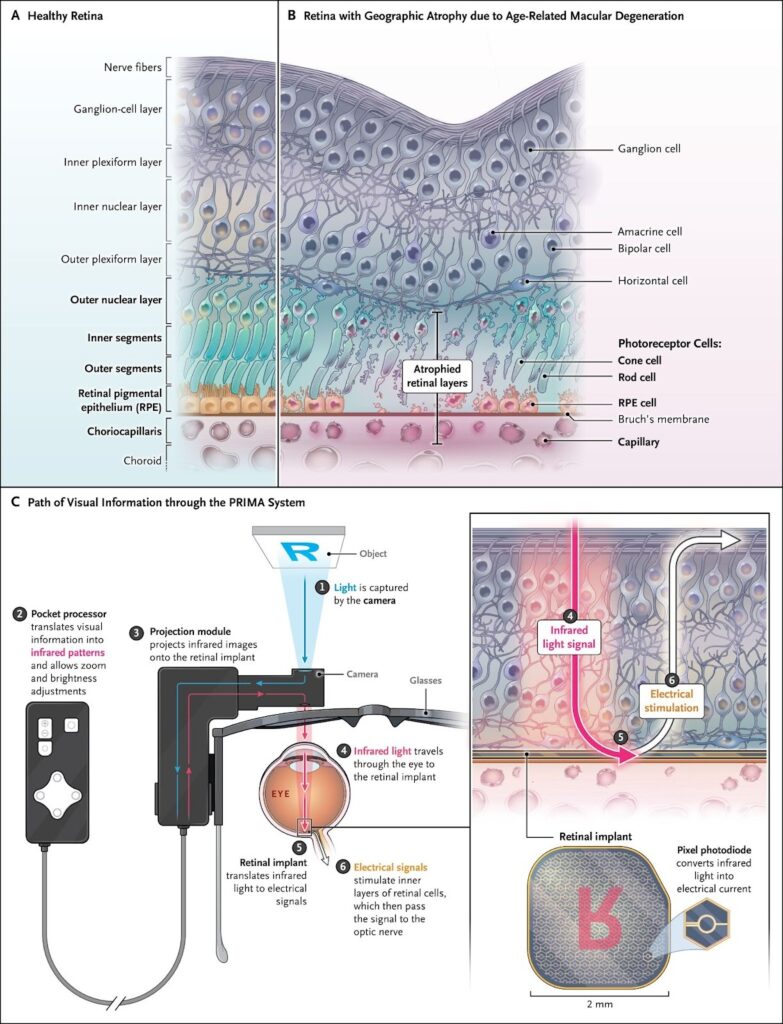
In a healthy retina, photoreceptors convert light into electrical signals that are processed by the inner retina and sent to the brain. In GA, photoreceptor loss blocks this process, creating an absolute scotoma (blind spot).2
The implant converts near-infrared light into electrical pulses that directly stimulate bipolar cells, reactivating the visual pathway.3
READ MORE: Ocular Imaging: Discovering Groundbreaking Studies that Stole the Spotlight at APVRS 2023
Safety: Always a concern
According to the study1, 19 out of 38 patients reported 26 serious adverse events (SAEs), considered related to the procedure or a combination of the procedure and device.1
- 21 SAEs (81%) occurred within two months post-surgery, of which 20 (95%) resolved within two months.
- 22 SAEs (85%) were classified as mild or moderate.
- 4 SAEs (15%) were severe (full-thickness macular hole, ocular hypertension, retinal detachment and proliferative vitreoretinopathy).
Also, OCT and fundus photography showed that the inner retinal structure in the atrophic area did not appear to have been altered by the subretinal placement of the implant.1
More importantly, the investigators noted that all serious adverse events related to the procedure or device had been prespecified in the risk analysis—and none were life-threatening. After reviewing these and other findings from the study, the data and safety monitoring board of said study determined that the benefits of the PRIMA system outweighed the risks associated with implantation.1
READ MORE: Seeing the Unseen: Adaptive Optics Enters the Clinical Arena at ARVO 2025
Relevance in current ophthalmic practice
For retina specialists, results of this study provides a promising treatment for patients with GA due to AMD.
The PRIMA system is wireless. The photovoltaic nature of the implant enables wireless operation combined with a straightforward technique.3-5 Procedure for Implantation uses the standard vitrectomy techniques, a familiar procedure that clinicians use.
The wireless design reduces the surgical risks while the thin implant integrates well with the retina without fixation hardware.5
The PRIMA glasses are transparent, providing patients with natural vision and prosthetic central vision simultaneously.3 Based on this study’s results, it seems to be a big step toward a truly restorative therapy for GA—a paradigm shift from “slow the loss” to “restore the light.”
And because the natural peripheral field is not affected, the patients’ spatial awareness remains functional, which is a major benefit to mobility and quality of life.1
READ MORE: Advancing the Management of Geographic Atrophy
Looking ahead
The study results demonstrated that the PRIMA system is not just a low-vision aid because optical magnifiers or implantable telescopes are just enlarging the image to use what’s left of the functioning retina.1 It looks more like that the PRIMA System is “restoring” the central activity of the retina that has expired. Compared to epiretinal implants, the PRIMA implant stimulates bipolar cells rather than ganglia—this preserves features of inner retinal signal processing.3
The future for PRIMA is looking even more exciting. Its wireless design allows for replacement with higher resolution next-generation implants or implantation of multiple arrays in a tiled pattern at the atrophic area with minimal incision. The authors emphasized though that no PRIMA implant has been explanted in any human patient.1
To validate the current (12-month) study results, secondary outcome measures are being assessed up to 36 months to observe the long-term performance and retinal integration of the system. If positive outcomes persist, it could become the first clinically viable solution for vision restoration in AMD-related geographic atrophy.
READ MORE: FDA Expands Label for Izervay in Geographic Atrophy Treatment
For patients who have long seen the world in shadow, this is quite literally a return to the light. For ophthalmologists, it serves as a reminder of how vast the possibilities in ophthalmology are—from diagnosing blindness to helping the blind see—and with these revolutionary breakthroughs, the once impossible goal of restoring vision to the blind may one day become reality.
Editor’s Note: This content is intended exclusively for healthcare professionals. It is not intended for the general public. Products or therapies discussed may not be registered or approved in all jurisdictions, including Singapore.
References
- Holz FG, Le Mer Y, Muqit MMK, et al. Subretinal Photovoltaic Implant to Restore Vision in Geographic Atrophy Due to AMD. N Engl J Med. 2025; [Published Oct 20, 2025; Epub ahead of print.]
- Fleckenstein M, Mitchell P, Freund KB, et al. The progression of geographic atrophy secondary to age-related macular degeneration. Ophthalmology. 2018;125:369-390.
- Palanker D, Le Mer Y, Mohand-Said S, Sahel JA. Simultaneous perception of prosthetic and natural vision in AMD patients. Nat Commun. 2022;13:513-513.
- Lorach H, Goetz G, Smith R, et al. Photovoltaic restoration of sight with high visual acuity. Nat Med. 2015;21:476-482.
- Palanker D, Le Mer Y, Mohand-Said S, Muqit M, Sahel JA. Photovoltaic Restoration of Central Vision in Atrophic Age-Related Macular Degeneration. Ophthalmology. 2020 Aug;127(8):1097-1104.