When glaucoma complicates the retina, the rulebook gets rewritten. Here’s how the experts adapt.
On Day 2 of the 18th Congress of the Asia-Pacific Vitreo-Retina Society (APVRS 2025), a dedicated session explored the management of glaucoma secondary to retinal disease. Led by Filipino glaucoma specialists, the symposium examined how retinal pathology can alter glaucoma progression, complicate monitoring and reshape both medical and surgical decision-making.
Chaired by Dr. Nilo Vincent Florcruz (Philippines) alongside Dr. Carlo Antonio Nasol (Philippines), the symposium focused on real-world clinical dilemmas that arise when retinal and glaucomatous damage overlap. Speakers consistently emphasized that secondary glaucoma associated with retinal disease demands flexibility beyond existing standard guidelines, with earlier referral, individualized management and closer subspecialty collaboration playing important roles .
READ MORE: Greening Eye Care: Sustainability Takes Center Stage at APVRS 2025
Monitoring progression when structures overlap
Dr. Maria De Guzman (Philippines) of Asian Hospital opened the session by addressing the challenge of identifying true glaucoma progression in eyes affected by retinal pathology. She explained that secondary glaucoma differs fundamentally from primary open-angle glaucoma, particularly in how intraocular pressure (IOP) elevations and associated damage evolve.
“Unlike the most common type of glaucoma, which is primary open angle glaucoma, we may be able to prevent or halt the progression of the mechanism of the IOP elevation when it comes to secondary glaucoma,” she noted.
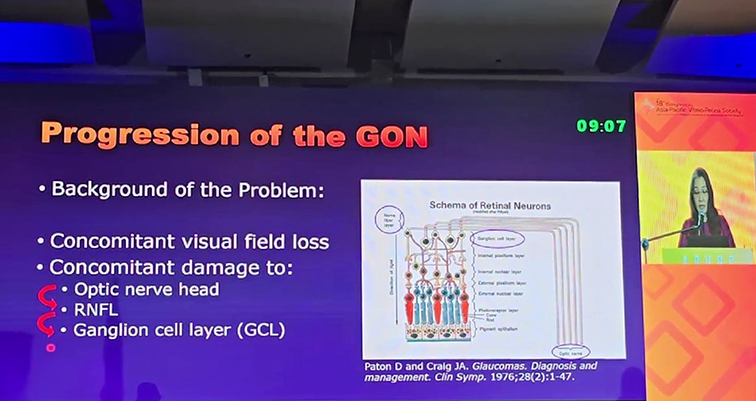
Dr. De Guzman emphasized that overlapping damage from coexisting retinal disease and glaucoma can complicate the interpretation of diagnostic testing. She further stressed that clinicians often see only the cumulative damage at a single point in time, which can obscure the true driver of disease progression.
“When we see our patient in the clinic, all we can see is the totality of the damage at that point in time. So, that’s our dilemma,” she said.
To address these challenges, Dr. De Guzman highlighted the importance of carefully timing diagnostic tests after acute IOP elevations and resetting baselines following significant retinal or pressure-related events.
READ MORE: All Eyes on Geographic Atrophy at APVRS 2025: Diagnostic Challenges and Scientific Advances
Setting the target IOP in glaucoma with co-existing retinal disease
Continuing the discussion, Dr. Christine Siguan Bell (Philippines) examined how retinal pathology reshapes the process of setting target IOP in patients with glaucoma. “Target IOP is an individualized range based on baseline IOP, severity and rate of glaucoma progression,” she explained.
While established guideline principles remain foundational, she emphasized that “retinal disease reduces visual reserve. It increases optic nerve vulnerability and limits the reliability of your OCT and visual field testing.”
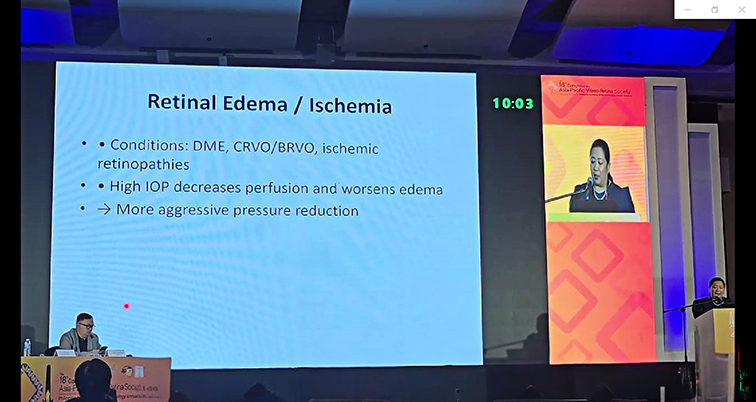
Dr. Bell further highlighted that repeated intravitreal and steroid exposure can contribute to IOP instability, often necessitating lower and more conservative pressure targets. Importantly, she stressed that IOP goals should not be static but reassessed regularly, as both glaucomatous and retinal conditions can evolve over time.
READ MORE: Retina Meets Rhythm: APVRS 2025 Opens with Lectures, Leaders and Filipino Flair
Anti-VEGF as a critical bridge in neovascular glaucoma
The session then turned to neovascular glaucoma, with Dr. Daryle Jason G. Yu (Philippines) describing the condition as a rapidly progressive disease driven by ischemic retinal pathology that ultimately leads to anterior segment damage.
“We all know that neovascular glaucoma results from a cascade of events moving from a posterior problem to an anterior structural failure,” he said.
From a glaucoma specialist’s perspective, Dr. Yu emphasized that anti-vascular endothelial growth factor (anti-VEGF) therapy plays an essential role. Not as a cure, but as a stabilizing measure that allows clinicians to intervene more effectively and tailor subsequent treatment.
He discussed how angle neovascularization following anti-VEGF therapy can “buy time” for clinicians, a window that is often critical.
“Why is this critical? Because historical filtration surgeries in these hot hemorrhagic eyes fail almost universally,” he explained. “Anti-VEGF is the necessary bridge that turns a highly vascular, inflamed eye into a quiet, cold one, making subsequent definitive treatment feasible. We must approach neovascular glaucoma as a…coordinated relay race.”
Dr. Yu concluded by emphasizing that while anti-VEGF is essential for short-term control of neovascular glaucoma, long-term success depends on sustained systemic management and close collaboration between glaucoma and retina specialists.
READ MORE: Frontline Femmes: Women Reshaping Retina at APVRS 2025
Surgical decision-making in uncontrolled neovascular glaucoma
Dr. Christopher Cyrille N. Cabrera (Phillipines) delivered the fourth talk, focusing on the surgical options available for uncontrolled neovascular glaucoma. He emphasized that, despite advances in surgical techniques and devices, outcomes remain variable.
“Neovascular glaucoma is actually one of the hardest glaucoma diseases to manage,” he said.
Dr. Cabrera explained that while trabeculectomy, glaucoma drainage devices and cyclodestructive procedures are all good options, no single approach guarantees complete success in every patient.
“There is still no universally superior procedure that we can choose,” he noted.
According to Dr. Cabrera, surgical decision-making must be highly individualized, taking into account disease severity, visual prognosis and surgical risk, particularly in eyes already compromised by retinal ischemia, inflammation and prior retinal interventions.
READ MORE: Retina 360 in the Pearl of the Orient: APVRS 2025 Begins
Managing glaucoma after retinal detachment surgery
Addressing glaucoma in eyes that have undergone retinal detachment (RD) surgery, Dr. Rainier Victor A. Covar (Philippines) highlighted the sustained risk of IOP elevation long after a retinal repair.
“Primary open angle glaucoma in eyes with RD has a four to 12 times higher risk compared to the general population and high myopia—which is a risk factor for retinal detachment—is also a risk factor for primary open angle glaucoma,” he explained.
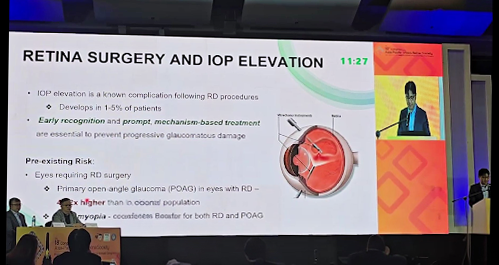
Dr. Covar stressed that this elevated risk extends well beyond the immediate postoperative period. “Lifelong glaucoma monitoring is mandatory for high risk patients due to the sustained nature of the risk,” he emphasized.
He also noted that conjunctival scarring and altered ocular anatomy often limit the success of traditional filtration surgery, making glaucoma drainage devices a more practical option in many of these complex cases.
READ MORE: Manila Spotlight: Insider Travel Tips and Must-See Attractions for APVRS 2025
Managing silicone oil-induced glaucoma
The final presentation was delivered by Dr. Maria Catherina Coronel Nasol (Philippines), who focused on glaucoma following pars plana vitrectomy with silicone oil tamponade.
“Silicone oil-induced glaucoma is becoming more common in countries and centers with poor access to health care and poor health seeking behaviors,” she noted.
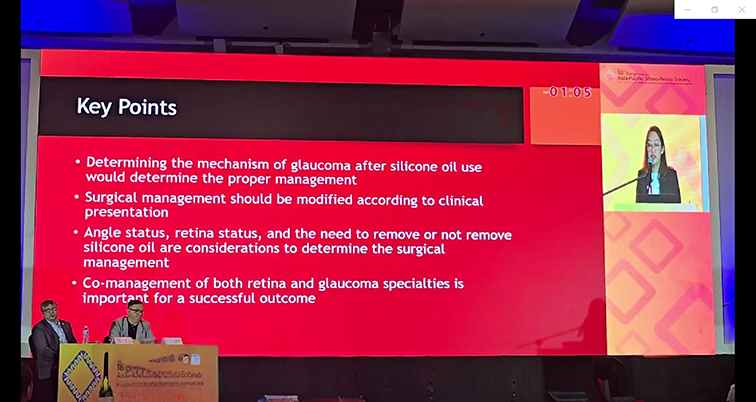
Dr. Coronel Nasol shared local clinical data that underscored the scale of the problem. “In our local study done in Cardinal Santos, the incidence of silicone oil-induced ocular hypertension is around 47.8%.”*
She emphasized that silicone oil-related glaucoma is highly variable in its underlying mechanisms and therefore requires individualized, mechanism-based management. Close collaboration between retina and glaucoma specialists, she stressed, is essential to prevent irreversible vision loss.
*Ge L, Su N, Fan W, et al. Risk factors for management of intraocular pressure elevation after vitrectomy combined with silicone oil tamponade. Int J Gen Med. 2024(17):447-456.
Editor’s Note: This content is intended exclusively for healthcare professionals. It is not intended for the general public. Products or therapies discussed may not be registered or approved in all jurisdictions, including Singapore. Reporting for this story took place during the 18th Congress of the Asia-Pacific Vitreo-Retina Society (APVRS 2025) from 12-14 December in Manila, Philippines.
