Sponsored by LKC Technologies
Vessels tell part of the story, but ERG spills the secrets. From uncovering preclinical dysfunction to predicting who’s headed for trouble, functional testing is stepping into the spotlight of DR management.
Diabetic retinopathy (DR) may be the quietest troublemaker in eye care, often advancing long before structural changes show up on imaging. By the time vascular abnormalities appear, the retinal dysfunction behind them may already be permanent.
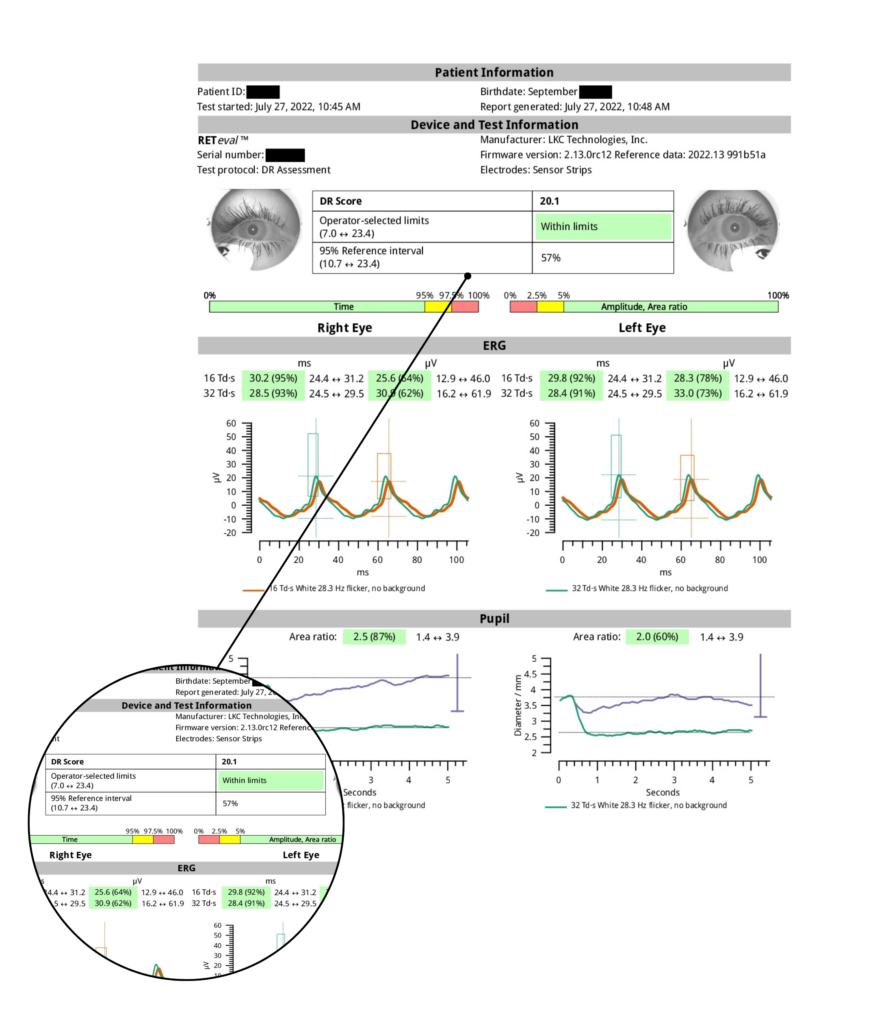
Functional testing with electroretinography (ERG), including the handheld RETeval™ (LKC Technologies; Maryland, USA) device, offers a way to catch this dysfunction sooner.1 As a portable, non-mydriatic ERG, RETeval delivers rapid, objective insight into retinal function without dilation. Growing evidence suggests that ERG can reveal preclinical changes and predict progression, positioning it as a potentially pivotal tool in the early detection and management of DR.
Associate Professor Dr. Dan Cao from Guangdong Provincial People’s Hospital (Guangzhou, China) described ERG as a powerful early-warning system for DR. Dr. Cao and her team have spent more than 15 years studying the disease. Their early work with optical coherence tomography angiography (OCTA) uncovered microaneurysms in patients whose fundus exams still appeared normal. This led them to ask whether visual function could detect trouble brewing even earlier. “We wanted to see if ERG changes can precede the obvious fundus changes,” she said.
Initially, they combined OCTA with standard ERG to evaluate a large cohort of diabetic patients.2 But the traditional five-step ERG protocol proved too time-consuming. Transitioning to the RETeval DR protocol allowed them to capture implicit time and other key indices in under five minutes, prompting the shift to the handheld ERG device.
Their findings showed that in the preclinical stage of DR—before any visible microaneurysms or retinal hemorrhages—patients already exhibited prolonged implicit time and reduced ERG responses.
“Additionally, when we looked at patients with different stages of non-proliferative diabetic retinopathy [NPDR], we found that once the disease progressed beyond moderate NPDR, the ERG implicit time was more sensitive than OCTA in detecting the progression of diabetic retinopathy,” she said.
In practice, Dr. Cao sees handheld ERG guiding earlier intervention. “I think if we perform the hand-held ERG test in patients every time they come to our clinic, and we see the score increasing or the implicit time prolonged—other than the retinal hemorrhage or macular edema—it indicates that the patient’s retinal function is declining,” she explained. “This allows us to intervene earlier, potentially performing laser treatment or administering anti-VEGF therapy before the disease reaches the end stage.”

A crystal ball for progression
Dr. Mitchell Brigell, consultant at Opus Genetics, Inc. (North Carolina, USA) echoed Dr. Cao’s sentiment and emphasized ERG’s predictive value in managing DR.
In a study published in Ophthalmology Science3 on June 2025, Dr. Brigell and colleagues analyzed data from a clinical trial that was initially designed to test a drug aimed at preventing DR progression. Although the drug was ineffective, the dataset was a gold mine.
Participants with good vision and mild to severe NPDR underwent baseline ultra-widefield fluorescein angiography (FA), OCTA and RETeval ERG procedures. The researchers then assessed which measurements best predicted progression to vision-threatening diabetic macular edema (DME) or proliferative DR over the course of one year.
“We were surprised and happy to see that the ERG was the most predictive of who was going to progress to vision-threatening complications. The effect was fairly large: if the ERG was positive (meaning it showed an abnormal score) the likelihood of progression over the year was 73%,” he said. “Whereas if the ERG was negative, it was only 27%. Although some characteristics of the angiography and OCTA images were also statistically significant, this shows that the ERG has a strong predictive value.”
The reason, Dr. Brigell noted, is because it’s becoming much clearer that DR is more than just a vascular disease. “There’s a neurodegeneration component related to hyperglycemia and abnormal retinal metabolism. With imaging modalities you’re just looking at the vasculature. With the ERG, you’re actually looking at the function of the neural retina.”
These insights directly inform risk stratification and treatment planning for patients with DR. ERG can help determine which patients with otherwise good vision are at high risk for progression and require more frequent monitoring. It also could impact decisions regarding which patients would benefit from early preventative treatment intervention. “If you could be better at predicting which patients are at high risk to progress, you can then offer them these treatment options with more assuredness that it’s going to help them,” he explained.
Referring to a 2020 Translational Vision Science & Technology study4, he added that combining ERG with the Diabetic Retinopathy Severity Scale (DRSS) “gives much more predictive value than either one alone.” Patients who appear structurally severe but have a negative ERG are often low risk and do not require frequent visits, whereas those with mild or moderate DR with a positive ERG warrant closer monitoring.
Dr. Brigell emphasized that the value of ERG lies in complementing—not replacing—structural imaging. “If you add ERG to your screening tests, you can better see who’s going to benefit from interventions and better predict who you should follow more closely or intervene earlier to prevent progression,” he noted. “ERG should be used along with imaging technologies to better manage the care of patients with diabetic retinopathy.”
RETeval in the clinic
Electrophysiology, once highly regarded in the 1990s, gradually fell out of routine practice as traditional systems were cumbersome, time-consuming, uncomfortable and largely confined to specialized teaching hospitals with long waiting lists. In contrast, RETeval ERG is portable, user- and patient-friendly, efficient and provides fast results.
“The RETeval device has transformed patient management and disease diagnosis,” emphasized Prof. Paulo Eduardo Stanga, ophthalmology professor at the University College London and founder of The Retina Clinic-London Ophthalmic Institute (London, UK).
“On an everyday basis, my patient can have electrophysiology—whether to diagnose an inherited retinal dystrophy or follow up ischemic changes in DR. In five minutes, we get results from both eyes and can objectively follow the stability or progression of retinal perfusion, stroke or retinal ischemia,” he said.
According to Prof. Stanga, RETeval is fundamental to multimodal assessment, adding rapid, objective electrophysiology to imaging and OCT without disrupting clinic flow. This enables comprehensive diagnosis at first consultation.
“RETeval streamlines care, eliminating repeated testing and multiple follow-ups…thus reducing system burden, and giving patients peace of mind. RETeval can directly change management,” shared Prof. Stanga. For example, detecting ischemia in a diabetic patient can immediately indicate further investigation—either with ultra-widefield OCTA or invasive fundus fluorescein angiography. ERG also helps confirm diagnoses in uveitis and inherited retinal dystrophies, guiding treatment decisions, clinical trial eligibility and support gene therapy.
In a nutshell, RETeval enables rapid, non-invasive functional assessment, complements imaging, guides early intervention and streamlines DR management. As Prof. Stanga advised, clinicians should be open to trying RETeval: “They’ll be very pleasantly surprised by how quick and easy it is to do the test and get the results, how cost-effective it can be, and how much it is going to support their clinics on a day-to-day basis.”
Editor’s Note: This content is intended exclusively for healthcare professionals. It is not intended for the general public. Products or therapies discussed may not be registered or approved in all jurisdictions, including Singapore.
References
- Zeng Y, Cao D, Yu H, et al. Early retinal neurovascular impairment in patients with diabetes without clinically detectable retinopathy. Br J Ophthalmol. 2019;103(12):1747-1752.
- Zeng Y, Cao D, Yang D, et al. Retinal vasculature-function correlation in non-proliferative diabetic retinopathy. Doc Ophthalmol. 2020;140(2):129-138.
- Davis CQ, Waheed NK, Brigell M. Predicting Progression to Vision-Threatening Complications in Diabetic Retinopathy. Ophthalmol Sci. 2025;5(6):100859.
- Brigell MG, Chiang B, Maa AY, Davis CQ. Enhancing Risk Assessment in Patients with Diabetic Retinopathy by Combining Measures of Retinal Function and Structure. Transl Vis Sci Technol. 2020;9(9):40.